Carotid artery disease
Carotid artery disease can be one of the most common causes of strokes caused by ischemia. In general, stroke can be defined as any brain injury resulting in:
- Loss of speech - aphasia
- Loss of strength - monoparesis/hemiplegia
- Loss of vision
- Loss of memory and coordination
75% of all strokes can be attributed to
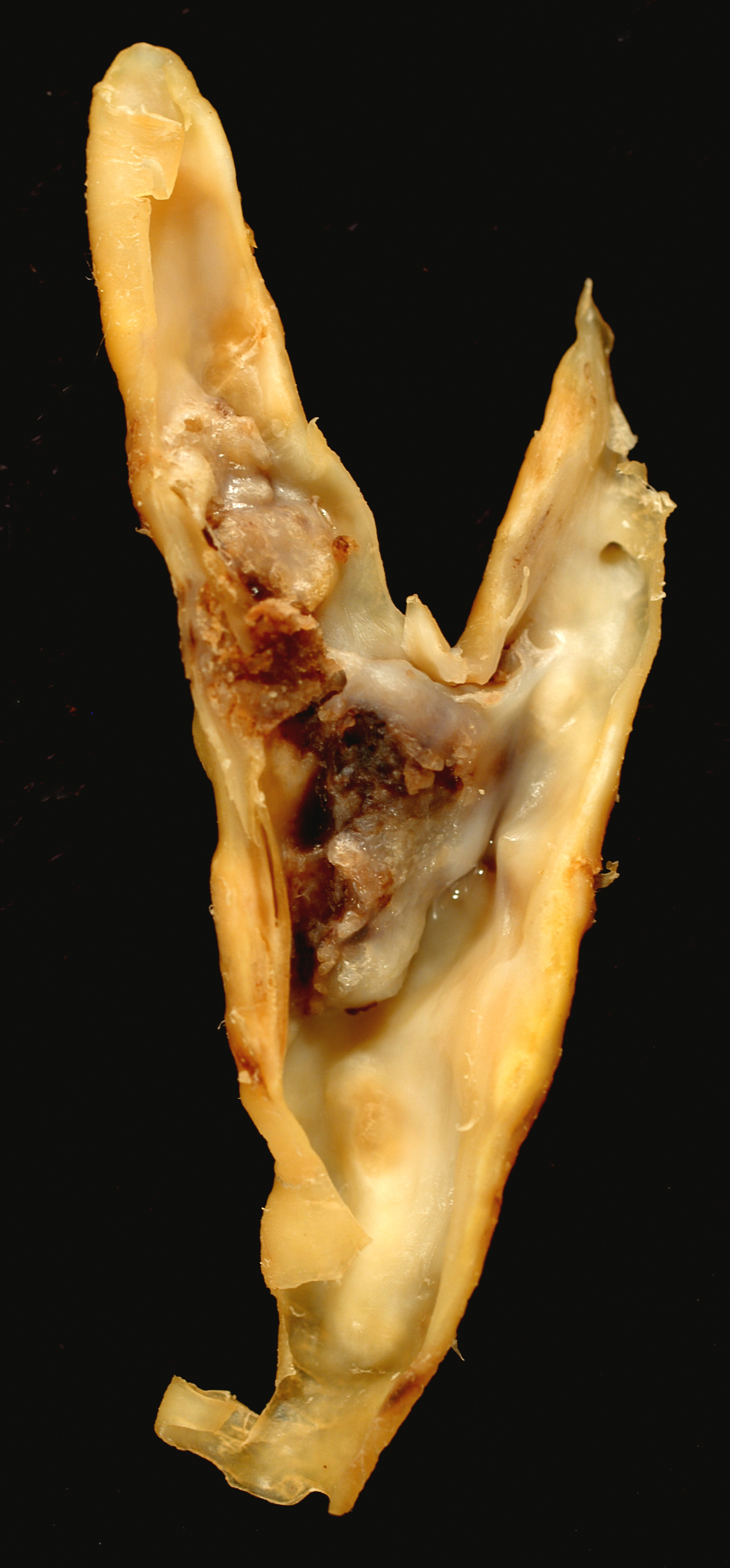
- Emboli from carotid artery plaques
- Carotid bifurcation disease is the most common cause of ischemic strokes and has 2 mechanisms:
- Carotid plaque discharge of microemboli into the cerebral circulation and resulting in a decreased cerebral perfusion
- Atherosclerosis of cerebral vessels leading to a total occlusion over time
- Carotid bifurcation disease is the most common cause of ischemic strokes and has 2 mechanisms:
- Emboli from the heart
- Common causes include atrial thrombus emboli from atrial fibrillation patients
- Embolization of a mural thrombi from the left ventricle in the presence of ventricular dysfunction
- Often seen after MI
- Diseased aortic and mitral valves can also result in small emboli
- Hypertension
- Hypertension can lead to a stroke through multiple mechanisms
- It can affect the small arteries of the brain resulting in micro-occlusions
- It can cause the rupture of the small arteries and lead to an intracerebral hemorrhage
- Hypertension can lead to a stroke through multiple mechanisms
Evaluating a patient
Diagnosing a stroke (or a TIA) in patients can be done in 2 means. Before we had wide imaging techniques such as CT and MRI, clinical diagnoses was the main and only way of diagnosing these conditions. With the advent of new imaging techniques anatomic and accurate diagnosis has been possible.
Clinical diagnosis (before CT and MRI)
- Transient ischemic attack (TIA)<24 hrs
- Cerebrovascular accident (CVA)>24 hrs
Anatomic diagnosis (Intracranial imaging)
- TIA = ischemic (but alive) tissue (not visible on imaging)

- Tisue infarction is avoided thanks to blood flow from other branches
- CVA = infarcted tissue (visible on CT and MRI)
- Irreversible death of brain tissue
History
Neurological symptoms are prognostic:
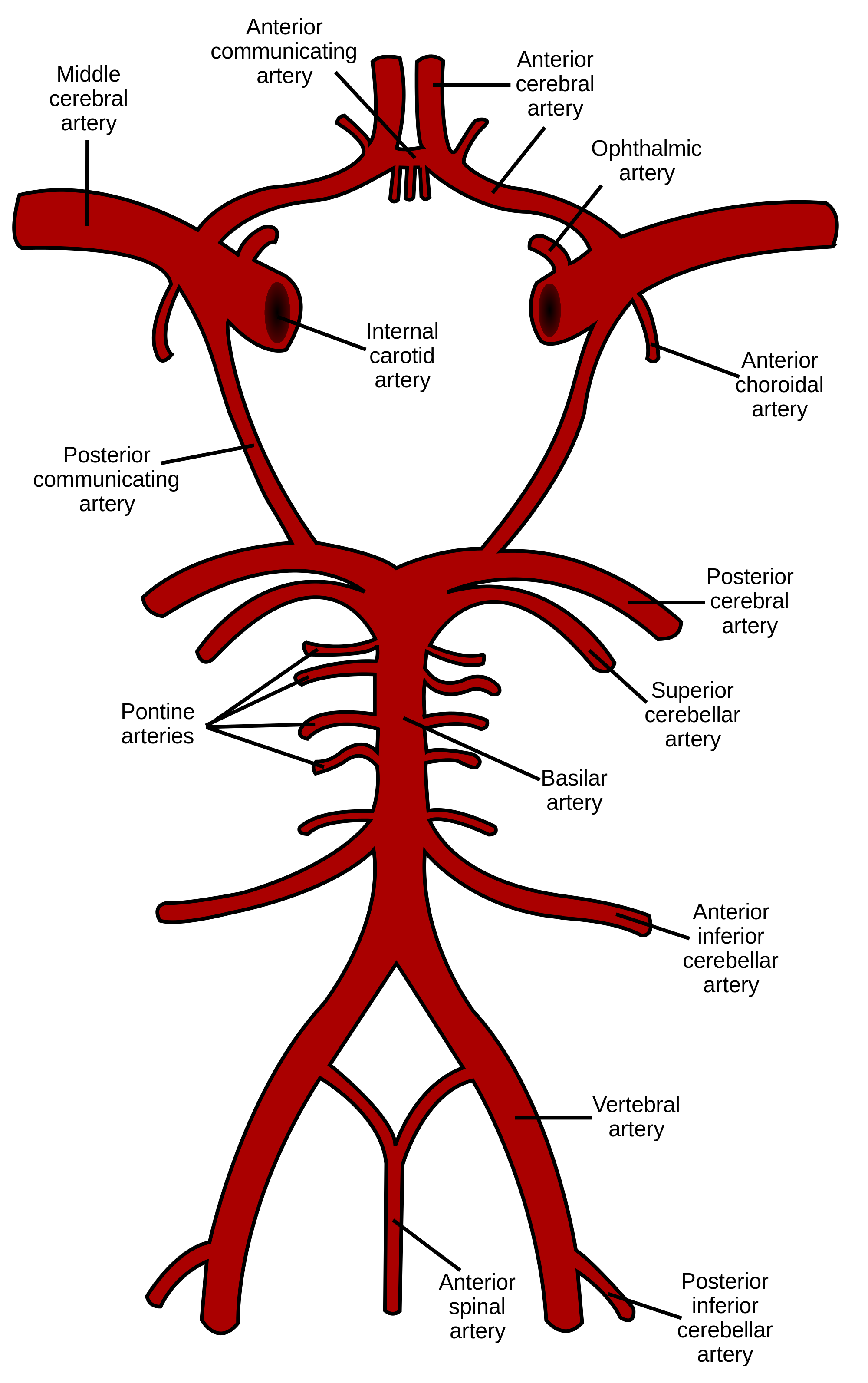
- Anterior circulation problem symptoms
- Internal carotid artery
- ACA
- MCA
- Ophthalmic artery to the eye
- Motor strip
- Contralateral mono/hemiplegia
- Contralateral mono/hemiparesis
- Sensory strip
- Sensory loss contralateral side
- Vision
- Ipsilateral monocular blindness
- Amaurosis fugax = transient monocular blindness
- These plaques can even be seen on fundoscopy of the retinal arteries and are known as Hollenhorst plaques - shown below
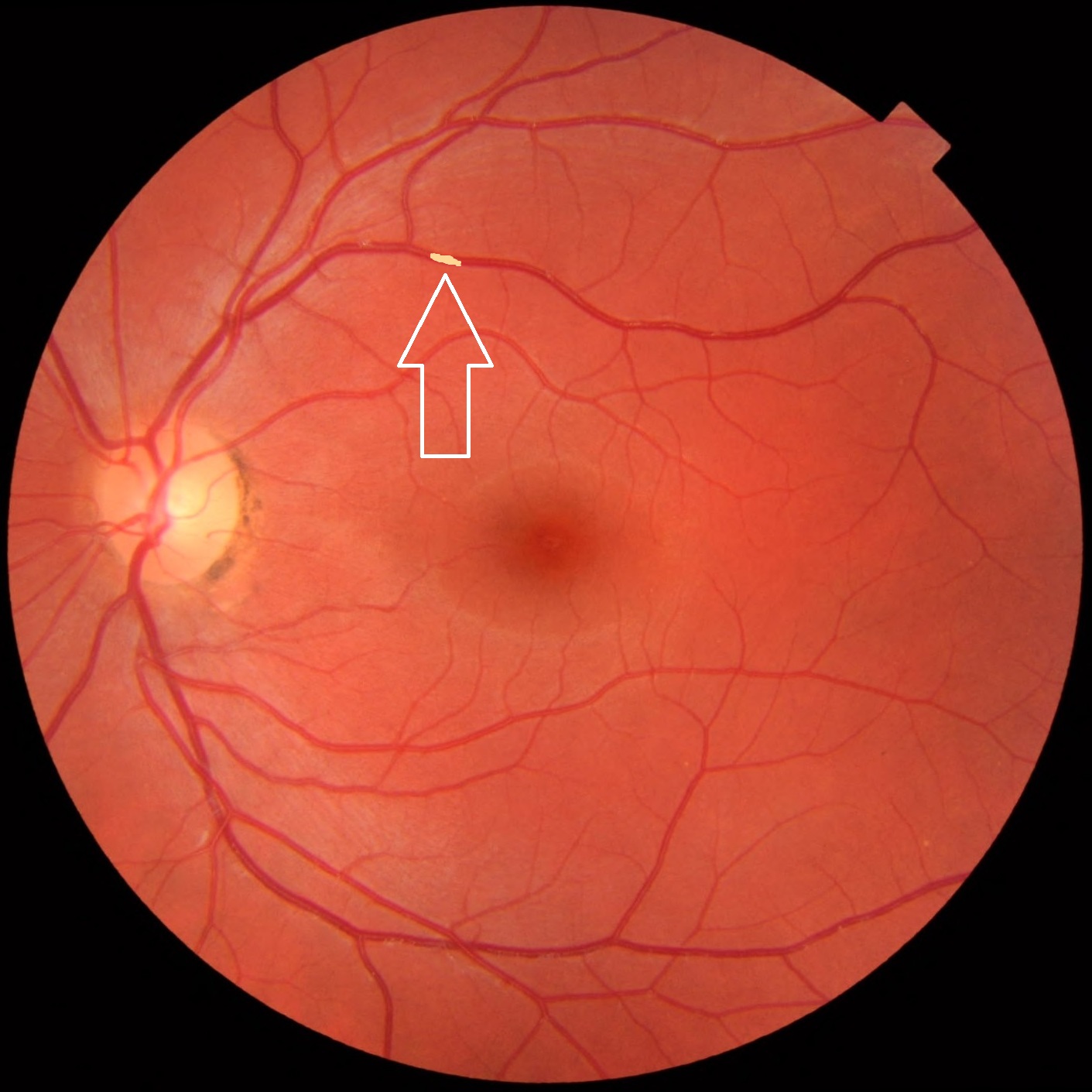
- Can turn into a permanent impaction
- Internal carotid artery
- Posterior circulation problem symptoms
- Vertebral and basilar arteries
- Ischemia of the brainstem, cranial nerves, and the cerebellum
- Symptoms
- Diplopia
- Ataxia
- Dysarthria - difficulty speaking
- Circumoral numbness
- Drop attack - The patient still conscious but drops to the ground due to cerebral hypoperfusion. The patient will remember the event
- Vertebral and basilar arteries
Cerebral ischemia can be temporary (TIA) recovering within 24 hours and permanent (CVA).
Physical exam
- Neurologic exam
- Ophthalmologic exam
- Focused vascular exam
- Carotid artery
- Feel carotid upstrokes gently to not disturb any more plaque
- Do not palpate both simultaneously
- Auscultate for bruits that indicate turbulent flow
- Ask the patient to hold their breath
- Auscultate at the angle of the mandible (most bifurcations happen here)
- Proximal subclavian and vertebral arteries
- Ask the patient to hold their breath
- Auscultate just above the clavicle
- Radial pulses
- Check both at the same time and assess for pulse lag
- This would indicate a proximal subclavian artery occlusion
- Check both at the same time and assess for pulse lag
- Check for AAA
- Relax the abdominal wall by bending the knees
- Bimanual palpation at the sides of the aorta at the level of the umbilicus - this will give an estimation of the width of the aorta
- If there is involuntary guarding, ask the patient to inhale and exhale, going deeper on each exhalation
- Renal and mesenteric vessels
- Auscultate for bruits
- Renal - under the costal margin
- Celiac, SMA and IMA bruits
- Auscultate for bruits
- Femoral arteries
- Palpate for groin aneurysms
- Just below the inguinal ligament
- Do not use groin crease or skin crease as landmarks
- The inguinal ligament is defined as the ligament from the anterior superior iliac spine to the pubic tubercle
- In obese patients, the inguinal ligament is usually higher than the soft tissue crease
- Just below the inguinal ligament
- Auscultate for bruits
- Palpate for groin aneurysms
- Popliteal artery
- Have the patient relax their knees completely
- Palpate for aneurysms
- Fetal arteries
- Dorsalis pedis pulses
- Posterior tibialis pulses
- Foot health
- Skin hair
- Nail health
- Skin health
- Carotid artery
Laboratory studies
- No specific lab examinations for carotid disease
- Instead, assess for other associated diseases
- Fasting serum glucose
- A1C
- Bun and Creatinine for renal insufficiency
- Lipid profile for multifocal disease
- Surgical risk
- Hematocrit and hemoglobin for anemia
- Platelet count
- Bun and creatinine because azotemic patients may have decreased platelet function
- Bleeding time
- Coagulation studies
- Prothrombin time for the extrinsic pathway
- Partial prothrombin time for the intrinsic pathway
- International normalized ratio (INR)
Imaging studies
There are multiple different modalities. All of them aim to determine the location of the lesion (useful for surgical planning) and the degree of stenosis (prognostic value).
- Modalities
- Conventional angiography
- Gold standard
- Transfemoral approach
- Invasive test
- Uses ionizing radiation
- Iodinated contrast - can make renal insufficiency worse
- Risk of stroke during diagnosis is 1%
-
Lesion location Degree of studies Risk factor Cerebral Angio +++ +++ ++++
-
- Duplex U/S
- Assessment of
- Spectral array
- Velocity
- Non-invasive
- May miss
- proximal and distal (to the bifurcation), intrathoracic and intracranial lesions
- Excellent for stenosis assessment but not for the location
-
Lesion location Degree of studies Risk factor Cerebral Angio +++ +++ ++++ Duplex + +++ None
-
- Assessment of
- MRA
- with or without gadolinium
- Non-invasive
- Non-toxic contrast
- May over grade stenosis
-
Lesion location Degree of studies Risk factor Cerebral Angio +++ +++ ++++ Duplex + +++ None MRA +++ + +
-
- CTA
- Newest
- Non-invasive
- Uses ionizing radiation
- IV iodinated contrast
- No risk of stroke because the contrast is not done through an intraarterial or an intraaortic catheter
-
Lesion location Degree of studies Risk factor Cerebral Angio +++ +++ ++++ Duplex + +++ None MRA +++ + + CTA +++ ++ ++
- Conventional angiography
Decision making
Carotid artery stenosis
- Defined as the ratio of the diameter of the narrowest residual lumen to the normal carotid artery diameter upstream
- Interestingly, a 50% diameter reduction of the carotid artery reduces the cross-section of the artery by 75%
- 75% diameter reduction of the carotid artery reduces the cross-sectional area by 94%
It is important to ask the patient what lead to the discovery of their carotid disease. This could come about as a result of neurological symptoms (TIA, stroke) or an incidental discovery from a screening test. This is important because it directly factors into whether or not a patient will benefit from surgical intervention. 2 Trials played an important role in the determination of these guidelines:
- Symptomatic patients
- Beneficial Effect of Carotid Endarterectomy in Symptomatic Patients with High-Grade Carotid Stenosis - NASCET trials
- Compared surgical and medical therapy in symptomatic patients with carotid artery stenosis
- Performed in the 1980s
- 659 patients
- For symptomatic patients with >70% stenosis at 2 years
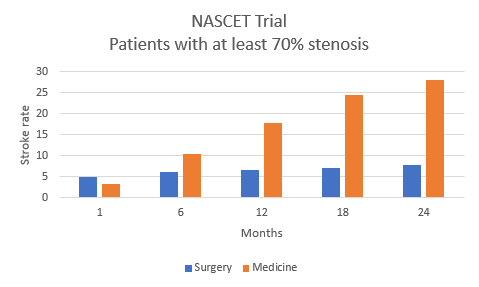
- The medically treated group had a progressively increasing stroke which reached 28% at 2 years
- The surgically treated group had an initial increased risk of stroke, but in the long term the rates of strokes were significantly reduced
- The study was terminated early because of its significant findings
- Symptomatic patients with >70% carotid stenosis and who are at a reasonable risk for surgery are advised to undergo carotid endarterectomy
- This study also looked at the outcomes based on the degree of stenosis
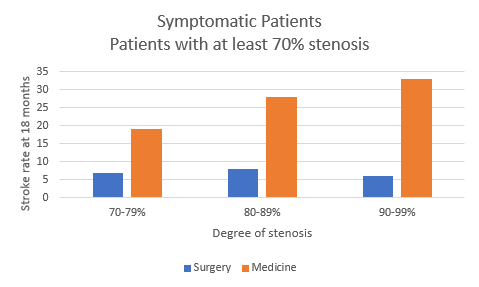
- Higher stenosis patients experienced higher rates of strokes
- Beneficial Effect of Carotid Endarterectomy in Symptomatic Patients with High-Grade Carotid Stenosis - NASCET trials
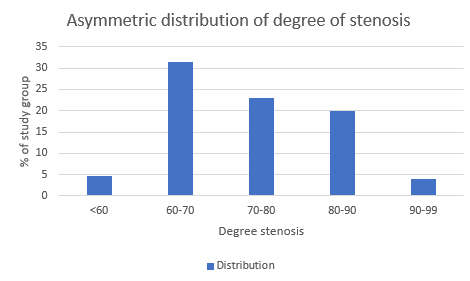
- Asymptomatic patients
- Endarterectomy for Asymptomatic Carotid Artery Stenosis - ACAS trials
- Compared surgical and medical therapy in asymptomatic patients with carotid artery stenosis
- Patients with >60% carotid stenosis who were asymptomatic
- Stroke rates at 5 years
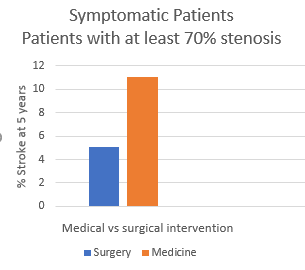
- If the patient had a stroke or a TIA the patients underwent immediate carotid endarterectomy (CEA)
- As a result, the medical arm of this study is not a true representation of the natural history of asymptomatic artery stenosis
- 146 of the 1659 enrolled patients were moved into the surgery group.
- Another concern about this study was the makeup of the severity of the patients
- The authors recommended surgery for patients with >60%.
- However, due to the aforementioned flaws, most clinicians recommend CEA to patients who are asymptomatic and >80% stenosis.
- Endarterectomy for Asymptomatic Carotid Artery Stenosis - ACAS trials
Complications of CEA
- Postoperative neurological deficit
- Can be multiple causes
- Low flow
- EEG and conscious patient monitoring
- Embolic complication
- Technical defect
- Stroke
- Thrombotic
- Technical defect
- Low flow
- Need to go back to the ER and place a shunt in
- Prevent further deficits
- Can be multiple causes
- Myocardial infarction
- Hemorrhage
- Consequences
- Increased intracervical pressure
- Decreased cervical venous return
- Vocal cord edema
- Tracheal deviation due to the hematoma
- The airway must be preserved
- Airway decompression
- Decompress all 3 layers
- Skin
- Platysma
- The deep layer of the deep cervical fascia
- Decompress all 3 layers
- Do not intubate first, decompress first
- Consequences
- Nerve injury
- Avoid
- Cauterization of the nerve
- Stretching
- Cutting
- Hematoma
- Nerves
- Glossopharyngeal nerve - CN 9 injury
- Difficulty swallowing
- Soft palate dysfunction
- Nasal regurgitation
- Vagus nerve - CN 10 injury
- Hoarseness due to the recurrent laryngeal nerve being affected
- Bilateral CEA can cause damage to both recurrent laryngeal nerves, leading to airway compromise
- Hypoglossal nerve - CN 12 injury
- Ipsilateral tongue deviation
- Marginal mandibular nerve injury
- Causes ipsilateral facial droop, not to be confused with a stroke
- Glossopharyngeal nerve - CN 9 injury
- Avoid
Long term follow-up is done with a duplex scan after 6 months and annually thereafter. Restenosis is measured with a duplex scan as well. Postoperatively check for cranial nerve injury as described above. Auscultate the neck for bruits on the ipsilateral side. This will give us a baseline understanding of the degree of turbulent flow.
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.