Colon cancer
A large proportion of colon cancers come from premalignant lesions (polyps) over multiple years (~10 years). A number of factors can increase the risk of developing colon cancer through this pathology:
- Age >50 years
- ETOH
- Smoking
- Obesity
- Processed red meats
The rest of the cancerous lesions are due to inflammation (Crohn's or Ulcerative Colitis) and genetics.
- The first step is medical therapy
- Some people fail medical therapy
- Types
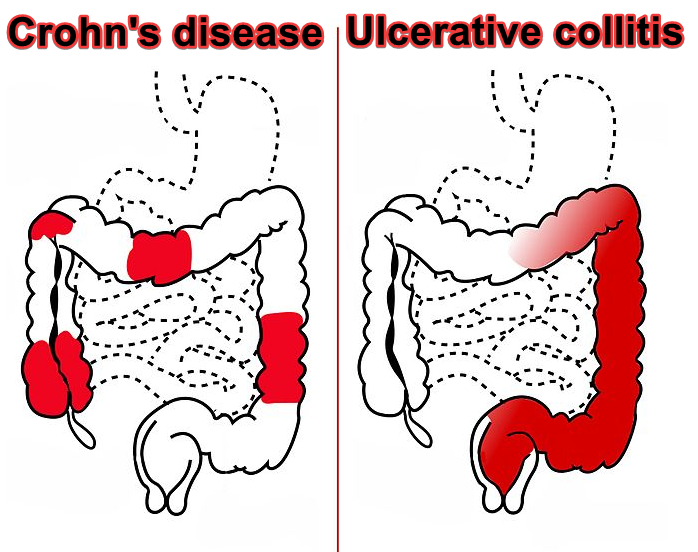
- Crohn's disease
- Transmural coverage - can form fistulas
- Signs
- Fecal soiling present
- Diagnosis
- Treatment
- Medical management only unless there is a fistula
- Fistulatomy
- Ulcerative colitis
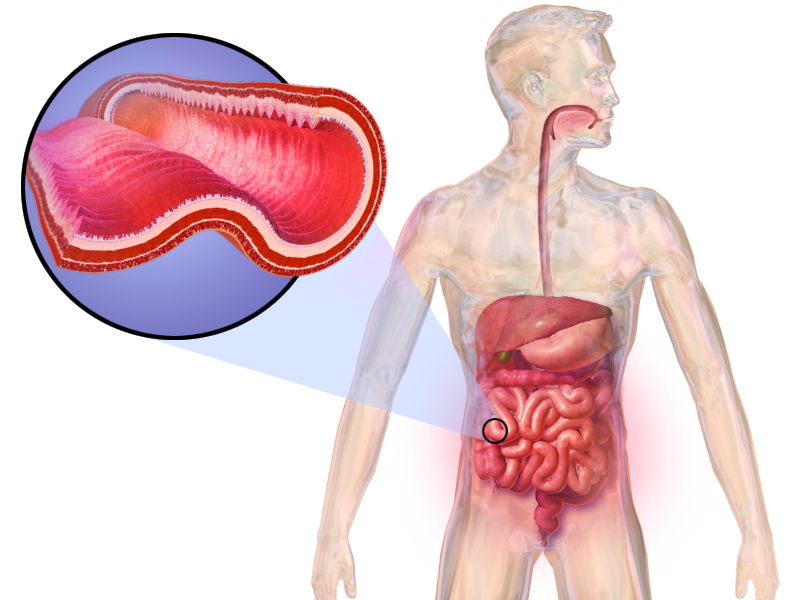
- Affects the superficial mucosa of the colon
- Continuous inflammation starting from the rectum - no skip lesions
- Signs
- Bloody bowel movements - will require a colonoscopy
- Rectal pain
- Weight loss
- Treatment
- Medical until 8 years
- 8 years after diagnosis = screening colonoscopy every year due to increased cancer risk
- Prophylactic colectomy will cure the disease
- Medical until 8 years
The most known genetic causes of bowel cancer are familial adenomatous polyposis (FAP) and Lynch syndrome. Below those and a few more genetic causes of colon cancer are discussed.
- FAP
- Pathophysiology
- Defect in the APC gene
- 1000s of polyps at a young age (in their 20s)
- These patients get colon cancer in their 30s and pass away by their 40s
- Prevention
- Prophylactic colectomy
- Early screening at age 10-15
- Pathophysiology
- Lynch syndrome - also known as hereditary non polyposis colorectal cancer (HNPCC)
- Pathophysiology
- Defect in the DNA mismatch repair systems
- No polyps involved, but will still get colorectal cancer
- Often multiple members of the family affected
- Remember the 3-2-1 rule
- 3 cancers (colon, endometrial or ovarian) in 2 generations and at least 1 premature age = Likely to be Lynch syndrome
- Remember the 3-2-1 rule
- Additionally these patients will also get
- Colon cancers
- Endmetrial cancers
- Ovarian cancers
- Pathophysiology
- Turcot's - (Remember: "turban" = head tumours)
- Pathophysiology
- Brain tumours and colon cancer
- Pathophysiology
- Gardner's
- Pathophysiology
- Jaw tumours and colon cancer
- Pathophysiology
- Peutz Jegherr
- Presentation - Freckles around the mouth
- Pathophysiology
- No colon cancer is present
- Small bowel cancer
- Will have to do endoscopy instead of colonoscopy
- Presentation - Freckles around the mouth
Presentation
- 3 common ways of presentation for most colon cancers are the followings:
- Found on an asymptomatic screen
- Regular screening age
- Age 50-75 (or 85 depending on the patient's mortality risk)
- Good polyps
- Pedunculated
- Tubular
- Small size
- Bad polyps
- Sessile
- Villous
- Large size
- Polyps in detail
-
Inflammatory Common in patients with IBD Low cancer risk Remove during colonoscopy Hyperplastic Small and located terminal to the colon Low cancer risk Remove during colonoscopy Tubular adenoma 70% of polyps are these Low risk if small in size Remove during colonoscopy
Increased follow up frequency required
Villous 15% of polyps are these Higher risk, especially if big in size Remove during colonoscopy
Larger polyps may require surgery
Serrated adenoma The remaining 10-15% of polyps are these Lead to 20-30% of the colon cancer cases Hard to see and remove with colonoscopy
-
- Regular screening age
- Iron deficiency anemia
- Concerning in men and post menopausal women
- Pencil thin stool or other signs of a mass

- Can have altered bowel habits (constipation and diarrhea)
- Can progress into a full obstruction Will have to do a colonoscopy with a biopsy
- Found on an asymptomatic screen
Diagnosis
- Colonoscopy with a biopsy
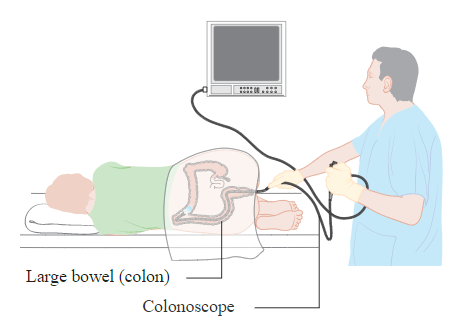
- Regular screening ages are 50-75
- After age 75, have to calculate the risks and benefits to the individual patient
- If nothing is found
- No risk
- Repeat every 10 years
- If a polyp is found
- Low risk
- 1-2 polyps, all of which are tubular with low grade dysplasia and <1cm in size
- Repeat every 5 years
- High risk
- >3 polyps or >1cm or villous type or high grade dysplasia
- Repeat every 1-3 years
- Mega risk
- >10 polyps
- Piecemeal sessile polyp present
- Repeat within 2-6 months
- Low risk
- Flexible sigmoidoscopy
- Ages 50-75
- Repeat every 5 years if nothing found
- Must be done with fetal occult blood testing (FOBT) every 3 years or every year
- FIT testing
- Better than FOBT
- CT colonography
- Less invasive but not as good as a colonoscopy screen
- Barium enema
- "Apple core" picture
- Not used very commonly anymore
- Staging of a confirmed cancer
- Pan CT - CT chest, abdo and pelvis
Treatment
- Resection
- Chemotherapy
- FOLFOX or FOLFIRI
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.



