Congestive heart failure
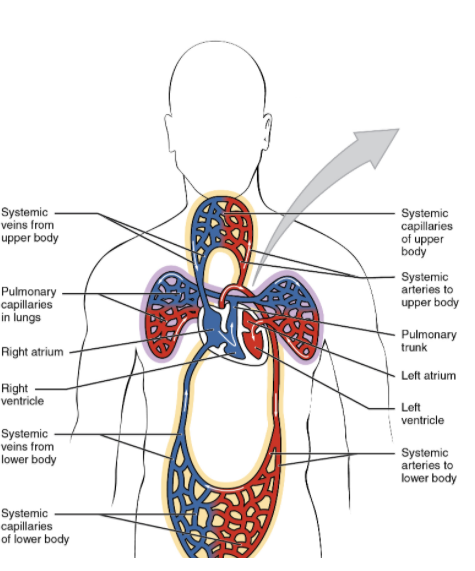
As we all know the blood flows from the left ventricle to the brain and the rest of the body. Then it is brought back by the venous system into the right atrium, right ventricle and the lungs. From the lungs, oxygenated blood travels into the left atrium and then the left ventricle to complete the cycle. In heart failure there is a problem with the heart, resulting in an ineffective cycle.
Picture 1. The 2 great cycles of blood in the human body
Right heart failure
Right sided heart failure is also known as diastolic heart failure and involves the failure of the right ventricle. As a result fluid backs up into the venous system. Acute right failure should be managed as hypertensive crisis.
Left heart failure
Left heart failure is also known as systolic heart failure and involves the weakening of the left ventricle. A weak left ventricle is not able to pump as efficiently and as a result, the blood is backed into the lungs initially. This eventually leads to a further back up into the right ventricle, right atrium and the venous system of the body.
Presentation
Considering that the left-sided heart failure involves the weakening of the heart, leading to the congestion of the lungs it is easy to understand the symptoms of CHF. The classic presentation includes orthopnea, paroxysmal nocturnal dyspnea and dyspnea on exertion. The presence of all 3 is highly specific for having CHF while having none of them almost guarantees the absence of heart failure. Additionally CHF patients will also present with reduced forward flow leading to altered mental state (exacerbation state). Since the right and left ventricles are connected through the lungs, a backup within the lungs will certainly be transferred to the right side of the body resulting in the symptoms of right-sided heart failure. These include peripheral edema, abdominal pain (due to the edema in the bowel), elevated JVP and elevated LFTs.
- Lungs
- Pulmonary crackles
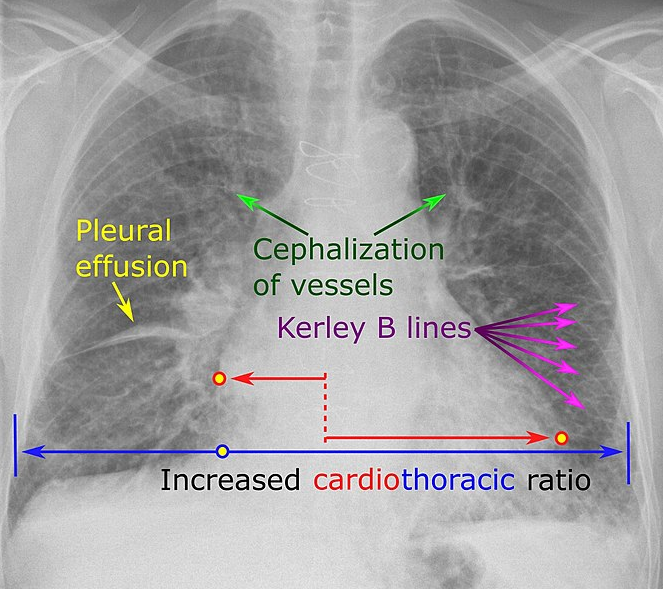
- Kerley B lines on U/S
- Pulmonary effusion
- Elevated JVP
- A sign of volume overload
- Associated with heart failure

- Edema
- Mostly peripheral
- Abdominal edema = abdominal pain
- Absorption of medicines and food is reduced
- Weight gain
- Cardiac
- S3 on auscultation
- Displacement of the PMI
- Changed level of consciousness
- As a result of reduced forward flow into the brain
- Cardiogenic shock
- Signs of tiredness
- As a result of reduced forward flow into the brain
- Renal issues
- As a result of reduced forward flow into the kidneys
- Decreased GFR
- Kidneys start to make renin
- Renin activates angiotensin ii
- Increased aldosterone production
- Sodium resorption
- Water resorption
- Increased preload as a result of the above 2
- Peripheral vasoconstriction
- Increased afterload
- Increased aldosterone production
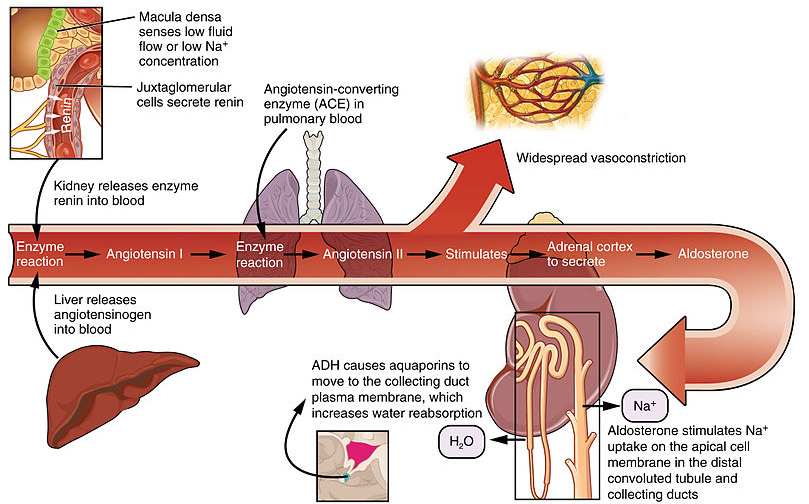
- As a result of reduced forward flow into the kidneys
Investigations
- BNP
- Best blood test for diagnosis
- <100 diagnosis excluded
- >500 highly likely for CHF
- Downfalls
- Obese patients will have low BMP even in a CHF state - false negatives
- Right heart strain due to chronic kidney disease, PE will elevate the BMP - false positives
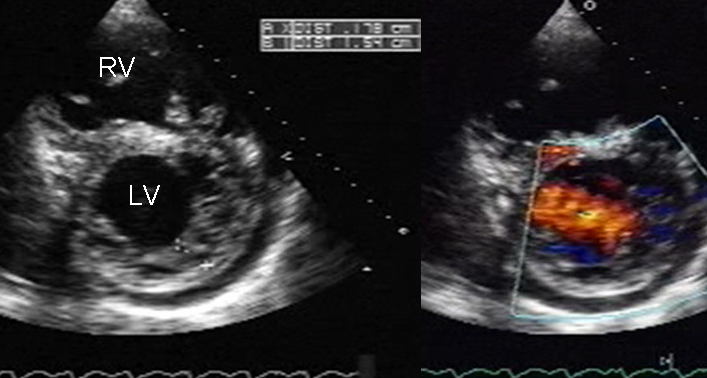
- Echocardiogram
- The best test to assess systolic vs diastolic heart failure
- Will show the ejection fraction
- Should be repeated during an exacerbation
- If the ejection fraction is low
- Left-sided heart catheter to check for ischemia
- ECG
- Can see old MIs and present arrhythmias
- Chest x-ray
- Can show fluid in the lungs and more
Diagnosis/Treatment
The New York heart association class (NYHA) is the scale used to categorize patients with heart failure into functional categories.
| Class | Description | Treatment |
|---|---|---|
| I | Completely asymptomatic. Can exercise at full capacity |
Beta-blocker = Arrhythmia reduction ACEi/ARB = Aldosterone reduction |
| II | Can exercise. Dyspnea starts at full exertion. Daily tasks cause no dyspnea |
Beta-blocker = Arrhythmia reduction ACEi/ARB = Aldosterone reduction Loop diuretics = Preload reduction |
| III | Daily tasks cause dyspnea. No dyspnea at rest |
Beta-blocker = Arrhythmia reduction ACEi/ARB = Aldosterone reduction Loop diuretics = Preload reduction Spironolactone/Bidil = Afterload reduction |
| IV | Dyspnea at rest |
Beta-blocker = Arrhythmia reduction ACEi/ARB = Aldosterone reduction Loop diuretics = Preload reduction Spironolactone/Bidil = Afterload reduction Milrinone/Dobutamine Left ventricular assist device (LVAD) Heart transplant |
Additionally, patients with CHF with an ischemic etiology should also be placed on aspirin (ASA) and a statin.
If the ejection fraction is below 35%, the patient will require a referral to an implantable cardioverter-defibrillator (AICD). This device is capable of performing cardioversion, defibrillation, and pacing of the heart, correcting most life-threatening arrhythmias.
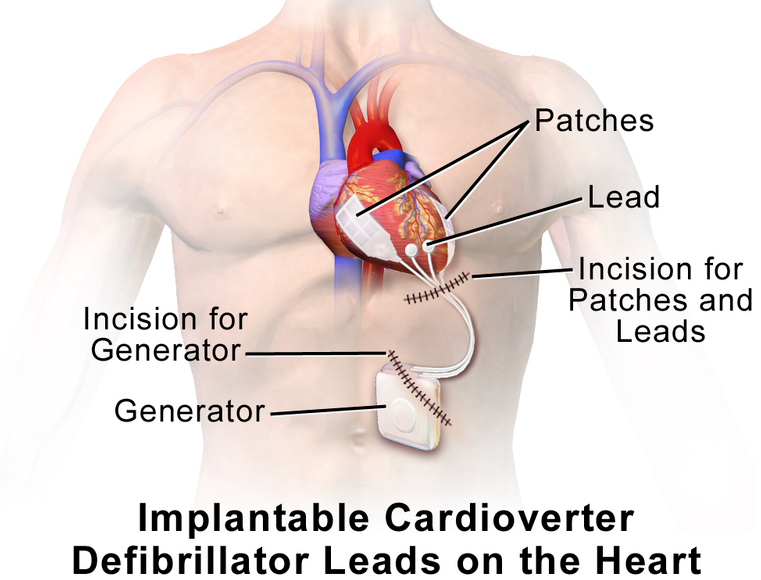
Picture 2. An implantable cardioverter-defibrillator is used if EF is <35%
NYHA class 4 patients are very sick and do not receive AICD, and instead are considered for constant Milrinone/Dobutamine infusions, LVAD and a heart transplant.
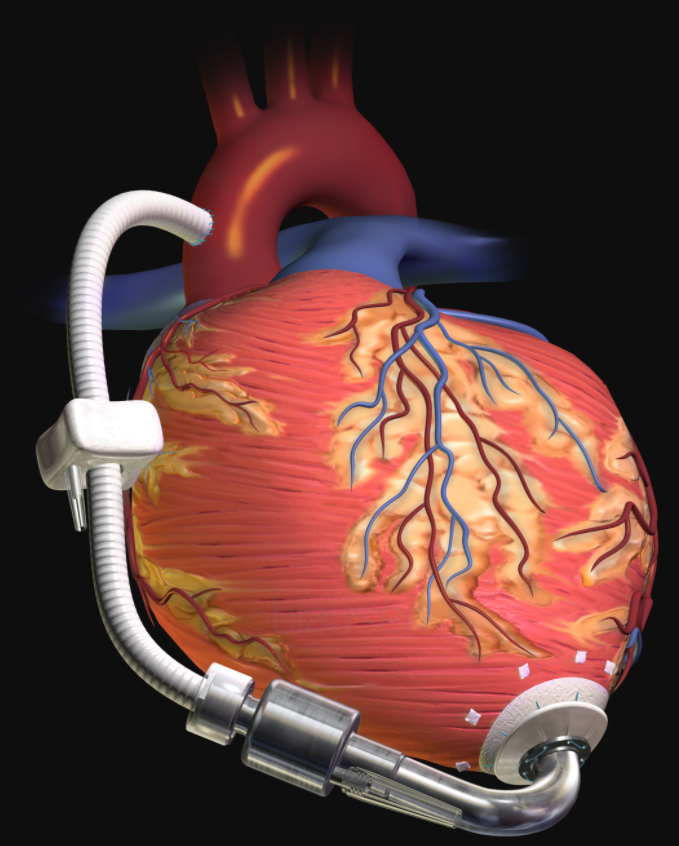
Picture 3. A left ventricular assist device is used temporarily before a heart transplant can take place
Lifestyle recommendations
- Sodium reduction
- < 2g salt daily
- < 2L water daily
- Weight checks daily
- One of the earliest changes of heart failure exacerbation
- If weight increases >5 pounds in 48 hours, double the dose of the diuretic

- Avoid NSAIDs
- Can worsen the renal blood flow
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.