DKA (Diabetic ketoacidosis)
Diabetic ketoacidosis which is commonly referred to as DKA, is a common initial presentation of young adults with type 1 diabetes mellitus. Type 1 Diabetes is caused by an autoimmune attack on the pancreas endocrine cells (alpha and beta) and directly results in low amounts of glucagon and insulin. Unlike in type 2 diabetes, these patients do not have resistance to insulin, instead they simply do not make enough insulin to manage their serum glucose levels.
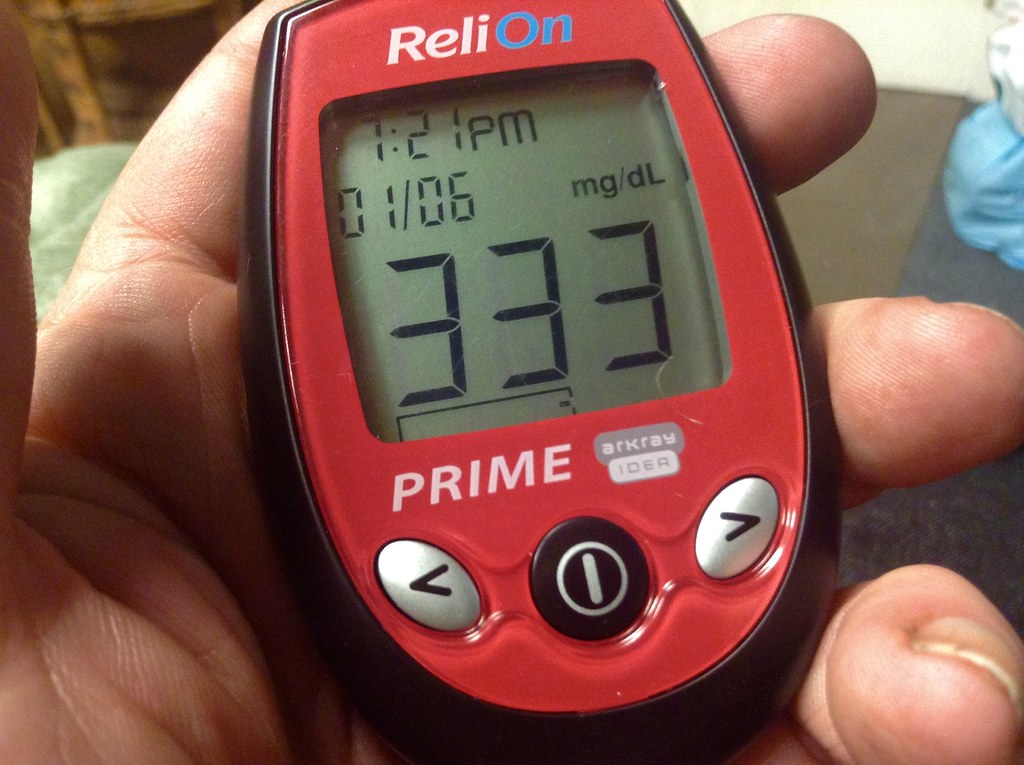
Diagram 1. Blood sugar can be very elevated in DKA and results in acidosis and dehydration.
One important fact to keep in mind is that DKA can occasionally also be seen in type 2 diabetes mellitus and should never be ruled out in these patients. Normally, insulin drives the uptake of glucose into the cells and inhibits lipolysis, glycogenolysis, ketogenesis, and tissue breakdown. When there is absolute (type 1 diabetes) or relative (type 2 diabetes, rarely experience DKA) deficiency in insulin, a state characterized by hyperglycemia and ketogenesis (DKA) can occur.
Causes
An easy way to memorize the causes of DKA is to memorize the 5 "I"s of DKA. These are the followings:
- Infection - most common external cause
- Often UTIs and respiratory infections
- Skin infections such as cellulitis
- Inappropriate sugar or alcohol intake
- Excess amounts of either
- Insulin use stopped - most common cause
- Noncompliance
- Can be unintentional
- Infant in uterus
- Pregnancy requires increased insulin requirement which can result in relative insulin deficiency
- Infarction
- MI, strokes, bowel ischemia
Presentation
The incidence of type 1 diabetes has a bimodal distribution. Patients often present for the first time in the early teens or in the late 50s. As such, most patients with DKA also have a similar incidence distribution graph. Unfortunately, given this age group and the symptoms, many new-onset diabetes patients presenting with DKA are misdiagnosed as having the flu. A patient who is known to have diabetes experiencing these symptoms should be presumed to be in DKA until proven otherwise.
Diagram 2. Incidence of type 1 diabetes. Bimodal graph.
Common presentation of DKA includes headaches, recurrent vomiting, inappropriate bradycardia, hypertension, Kussmaul respiration, irritation, lethargy, cranial nerve palsies (CN 6) and abnormal pupillary response. Most of these symptoms are nonspecific and require a high suspicion of DKA and appropriate workup for diagnosis. Kussmaul breathing is a respiratory compensatory mechanism for metabolic acidosis. The body tries to blow off CO2 and reduce the acidity of the blood. One interesting symptom of DKA is described as fruity breath which comes from ketones (acetone specifically).
Management and investigations
Giving IV fluids to these patients is essential due to the degree of dehydration. IV fluids lower the concentration of glucose but do not suppress the lipolysis and ketogenesis. The usual IV bolus fluid for DKA in pediatric patients is 10ml/kg of normal saline. Once an IV catheter has been established, the following labs are ordered:
- Blood glucose
- Elevated glucose
- Lytes
- Falsely elevated or normal potassium because acidosis pushes H+ ions into the cells and pushes positively charged K+ ions into the serum
- Total body potassium is depleted from the kidneys as more and more potassium is pushed into the serum
- Decreased serum sodium due to high glucose (we need to correct the sodium levels)
- Falsely elevated or normal potassium because acidosis pushes H+ ions into the cells and pushes positively charged K+ ions into the serum
- Blood gas
- Decreased = acidic blood pH
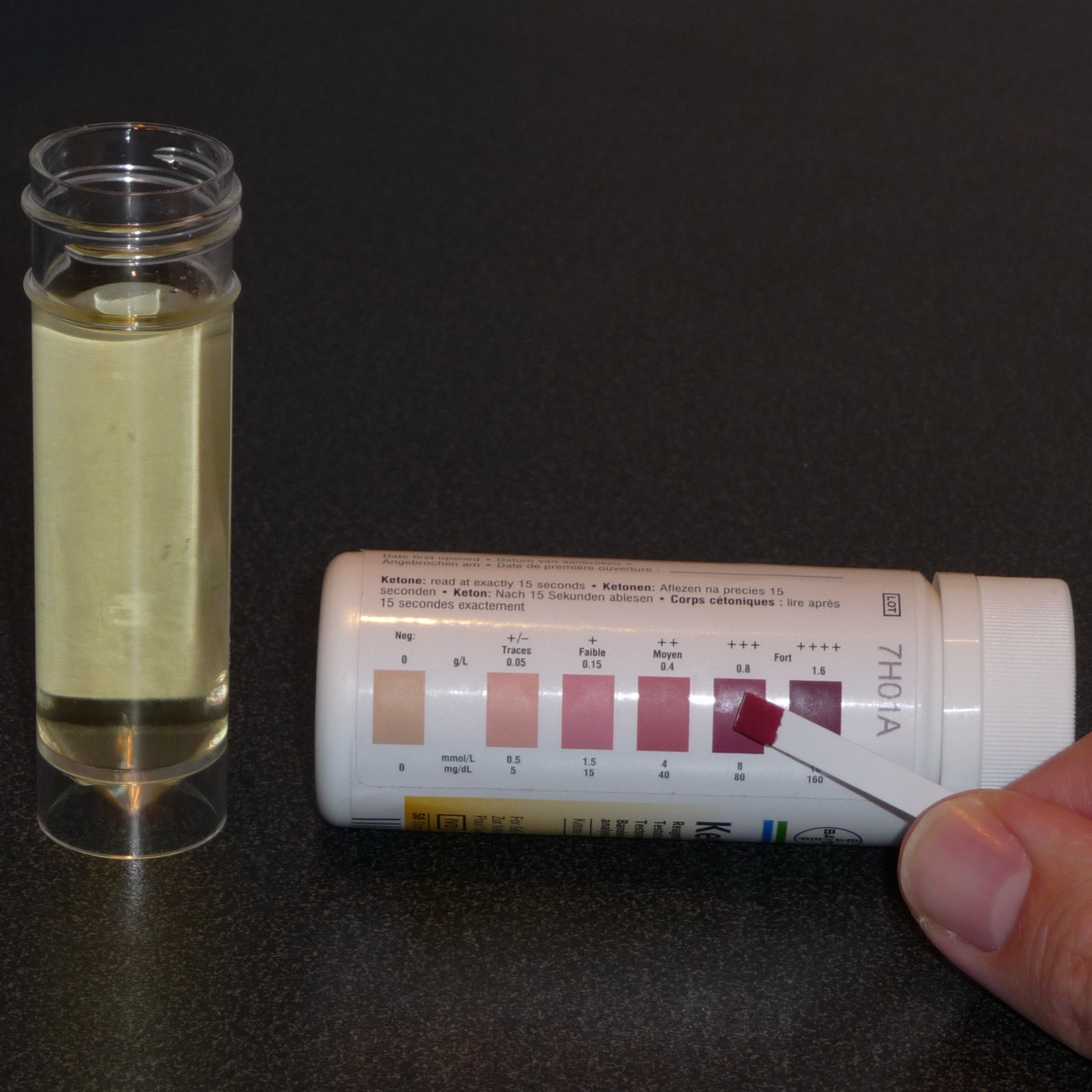
- Urinalysis
- Urine ketones detected
- Other markers
- Decreased bicarbonate level due to acidosis
- Increased creatinine due to hypovolemia
- Elevated anion gap acidosis
- Recall MUDPILES for causes of increased anion gap acidosis
- Methanol
- Uremia
- DKA
- Paracetamol = Tylenol
- Isoniazid (TB antibiotic), iron
- Lactic acidosis
- Ethanol or ethylene glycol (antifreeze)
- Salicylates
- Anion gap = Serum sodium - bicarbonate - chloride
- Any value above 12 is considered abnormal
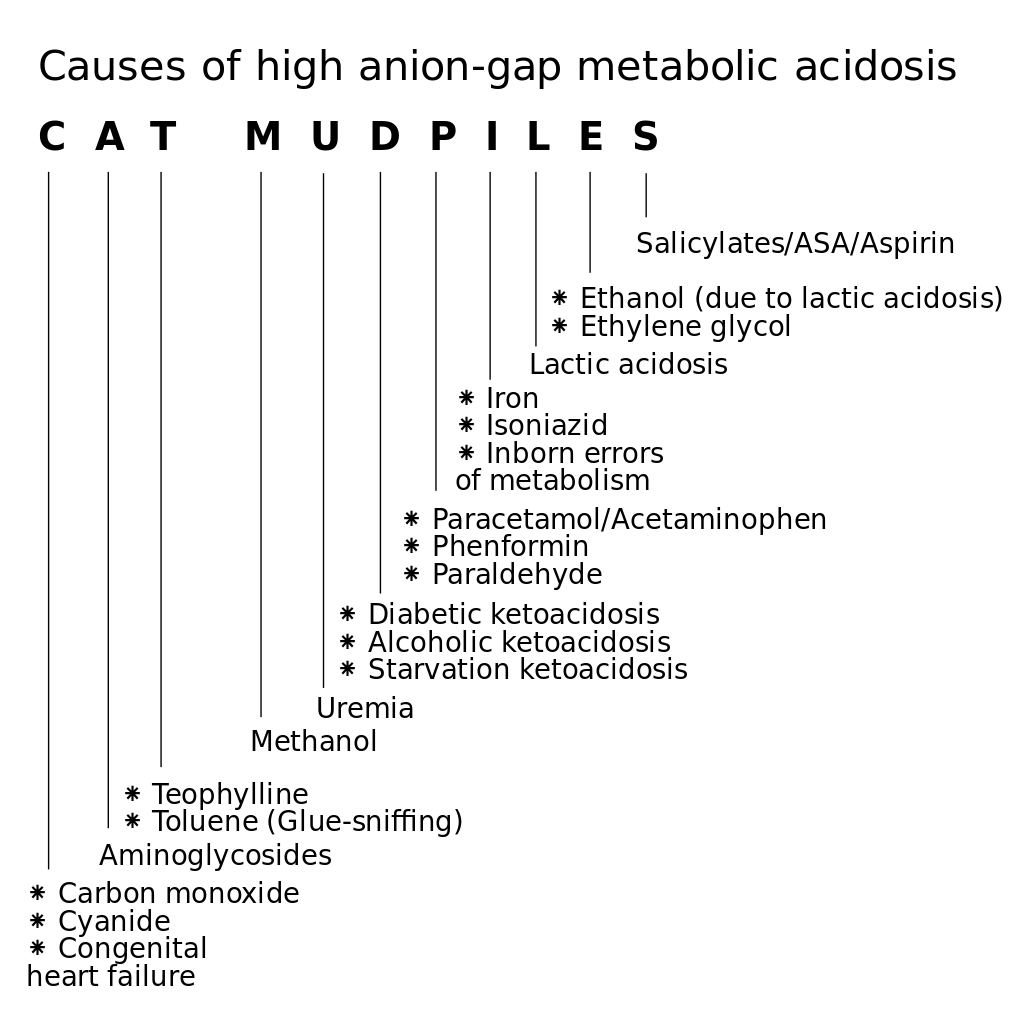
- Recall MUDPILES for causes of increased anion gap acidosis
Once the diagnosis of DKA is made the patient will need insulin injection, to stop and reverse the effects of ketogenesis and lipolysis.
- Insulin is started at 0.1 units/kg/hr after checking patients blood for serum potassium (never start insulin in a hypokalemic patient, infuse potassium first)
- Glucose levels should be monitored every 30-60 minutes
- Bicarbonate used to be administered to reverse the metabolic acidosis but is no longer recommended due to a high rate of cerebral edema and paradoxical CNS acidosis.
- As the acidosis is corrected, serum potassium will drop because potassium ions start to move into the cells (which are potassium depleted in DKA)
- Potassium added to the IV fluids as long as the levels are normal or low because a drop is expected during insulin administration
Admission to the hospital
Routine care for pediatric DKA patients is hospital admission with the following steps:
- Management of dehydration
- 10ml/kg bolus in DKA (20ml/kg in other cardiovascularly healthy patients) to make up for deficit fluid
- E.g for a patient weighing 32 kgs: bolus fluid=10ml/kg*32kg=320ml
- Bolus fluids are usually administered over 24-48 hour
- 4-2-1 rule for maintenance fluids
- Measure the patient's weight
- For the first 10 kg, 4ml/kg/hr = 40ml/hr
- For the second 10kg, 2ml/kg/hr = 20ml/hr
- For the third and subsequent 10kg, 1ml/kg/hr=10ml/hr
- E.g. for a patient weighing 32 kgs = 40ml+20ml+10ml+2ml=72ml/hr
- Ongoing loss replacement
- Vomiting
- Diarrhea
- NG tubes
- 10ml/kg bolus in DKA (20ml/kg in other cardiovascularly healthy patients) to make up for deficit fluid
- 10% dextrose administration
- This is needed because of acidosis and total body hypokalemia
- Insulin infusion normalizes the blood glucose, acidosis and initiates cell uptake of potassium
- However, acidosis and potassium uptake may take longer to normalize than blood glucose
- This may result in blood glucose dropping below normal
- 10% IV dextrose serves to maintain adequate serum blood glucose while the acidosis is reversed and potassium is driven into the cells (this will avoid a life-threatening condition which is hypokalemic-induced arrhythmia)
Below table 1 summarizes the list of orders that need to be followed after admission.
| NPO | Until blood sugar normalizes and all symptoms are resolved |
| Insulin infusion | Continue until acidosis is resolved |
| Serum glucose every 30-60 minutes | |
| Serum electrolytes every 60 minutes | Because serum electrolytes such as phosphorus and potassium will drop as they are driven into the cells |
| Hydration status monitoring | Prevent dehydration |
| Venous blood gas for pH | Metabolic acidosis reversal |
| Urinalysis for ketones | Should decrease with treatment |
| Neuro status check | Recognize early signs of cerebral edema |
| Monitor vitals | |
With appropriate inpatient management, many of these patients are back to normal within a short period of time and do not experience any long term complications. It is important to prevent the recurrence of DKA by educating the patient on keeping their glucose levels in the safe range and learn to recognize symptoms early.
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.
