Intra-uterine growth restriction (IUGR)
This is a fetal growth abnormality that occurs in ~5% of the obstetric population and one that is also known as fetal growth restriction (FGR), small for gestational age (SGA) and low birth weight (LBW) and describes small babies. Usually FGR and IUGR are terms that apply to fetuses in the uterus while LBW and SGA refer to babies who are low weight at the time of delivery. The definition of all these conditions includes a baby that is <10th percentile for a given gestational age.
Classification
IUGR can be classified as symmetric or asymmetric IUGR.
- Symmetric
- These make up 20-30% of all IUGR cases
- All fetal organs are decreased in size proportional to the fetal growth restriction
- Usually due to an earlier insult (hence affecting multiple systems)
- Asymmetric
- Relatively greater deficit in abdominal circumference [compared to head circumference] which is mostly made of of the liver and subcutaneous fat pad
- Fetuses that cannot get enough blood, prioritize the blood flow into the vital organs (brain, heart, placenta)
- As a result, non-vital organs (lungs, skin, kidneys) are underdeveloped
- Usually presents with head sparing (normal head circumference)
- Abdominal circumference <2.5th percentile in IUGR has 95% sensitivity in asymmetric IUGR compared to head circumference
Diagnosis
Estimating the fetal size prior to delivery is absolutely critical in diagnosing this condition early.
- Symphysis fundal height (SFH)
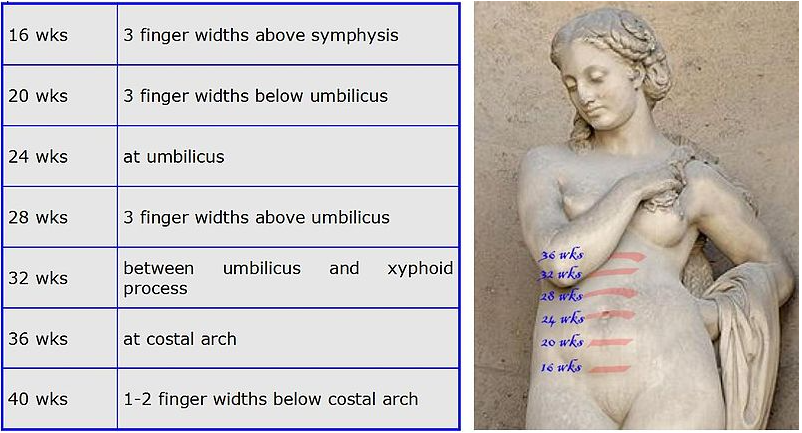
- Inexpensive way of estimating the gestational age
- Over 22 weeks of gestation the distance from the pubic symphysis to the top of the fundus estimates the gestational age in weeks
- A discrepancy of 2-3 cms can indicate fetal growth abnormality (sensitivity 28-86%)
- Ultrasound
- Measures the biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), femur length
- Margin of error
- 1 week up to 20 weeks gestation
- 2 weeks 20-36 weeks gestation
- 3 weeks over 36 weeks gestation
- Signs
- Oligohydramnios
- If the fetus is receiving limited blood the kidney perfusion will go down which can result in less than normal amount of fetal urine production/amniotic fluid
- Abnormal waveform in maternal and fetal blood vessels
- Oligohydramnios
Etiologies
Etiologies of IUGR are due to 3 different factors involved: the fetus, the mother and the placenta
| Fetal causes | Placental causes | Maternal causes |
|---|---|---|
|
Chromosomal (trisomy 13 and 18) Congenital Infectious Multiple gestations: twins, triplets Renal disease |
Infarcts Abnormal invasion into the uterine wall Abnormal cord insertion Tumours |
Nutritional Genetic Renal disease GDM Cardiovascular disease Environmental: smoking, EToH, drugs |
In general, chromosomal and infectious fetal causes tend to affect the fetus globally and result in symmetric IUGR.
Diagnosis
The best way to diagnose IUGR is in the antenatal period with an U/S scan.
Macrosomia

This term is used t describe an infant with excessive mass. Birth weight greater than 90th percentile or greater than 4000-4500g (variable due to race and neonatal sex).
|
Risk factor |
|---|
|
Diabetes - hyperglycemia in the fetus increases the amount of insulin, insulin-like growth hormone leading to a big fetus Large size of parents - maternal obesity Multiparity Maternal age Male fetus Previous macrosomia Race and ethnicity |
Diagnosis
It can be difficult to make an accurate measurement of the fetus. Both the SFA and the U/S results are used. SFH >2 cm than the expected gestational age should prompt an U/S scan. Increasing gestational age and maternal diabetes can make the error bars of U/S even wider for macrosomia.
The definitive diagnosis is made retrospectively, once a delivery is made and the baby has a weight measured.
Complications
- Maternal
- Perineal, vaginal and cervical lacerations
- Higher risk of a C-section
- Higher risk of infection, bleeding damage to the adjacent organs
- Risk of anesthesia
- Fetal
- Shoulder dystocia risk increased
- Can lead to brachial plexus injury, hypoxia, death
- Shoulder dystocia risk increased
- Neonatal
- Higher risk of hypoglycemia
- Higher risk of polycythemia
- Electrolyte instabilities
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.
