Gastroesophageal reflux disease (GERD)
GERD is a disorder of acid injury to the esophagus causing esophagitis. An incompetent lower esophageal sphincter (LES) is central in allowing this to happen.
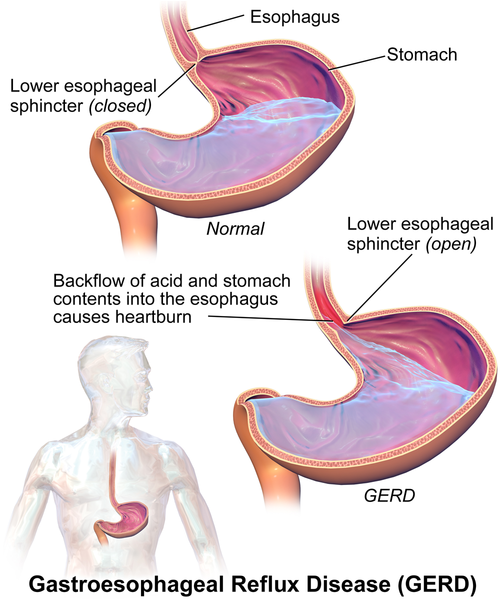
Pathophysiology
The acid from the stomach constantly burns the lower esophagus, causing constant inflammation. This leads the normal esophagus to undergo metaplasia and turn into columnar epithelium (similar to the duodenum). This is known as Barret's esophagus.
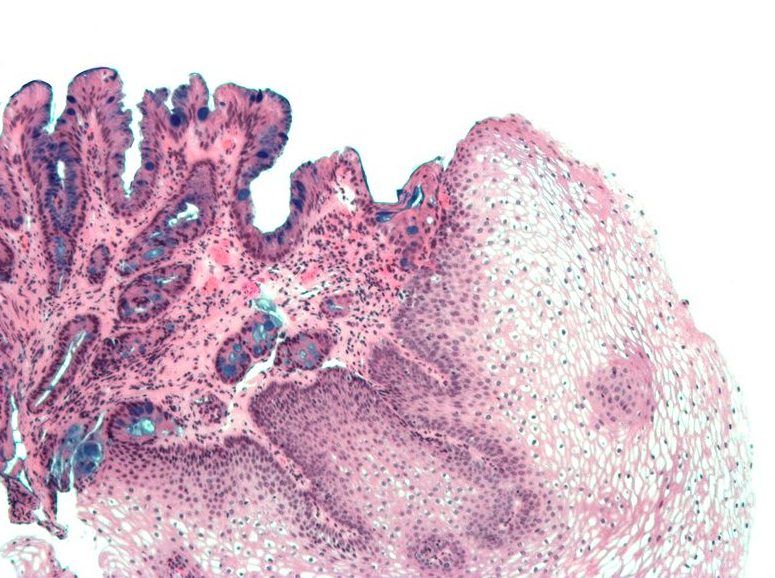
Picture 1. Metaplasia appears blue with the histology staining (alcian blue)
Barret's esophagus is a more durable tissue to the acid than the normal esophageal mucosa and patients can even feel better after this metaplasia takes place. The problem is that this new metaplastic tissue is at a 30-50 times increased risk to turn into dysplastic tissue, a precursor to adenocarcinoma.
Symptoms
- Typical symptoms
- Non-radiating, burning chest pain
- Worsened with lying down and better with standing
- Worsened by spicy and acidic foods
- Alleviated by antacids
- Atypical symptoms
- Voice hoarseness
- Coughing
- Nighttime asthma
Diagnosis
The diagnosis of this disorder in the absence of red flags starts with a trial of treatment. Start the patient on treatment for 6 weeks:
- If no red flags present
- PPIs for 6 weeks
- Better than H2 blockers and placebo
- Lifestyle changes for 6 weeks
- Avoid special foods such as chocolate, alcohol, peppermint

- Avoid lying down within 3 hours of eating
- Put up the head of the bed
- If the previous 2 steps are ineffective
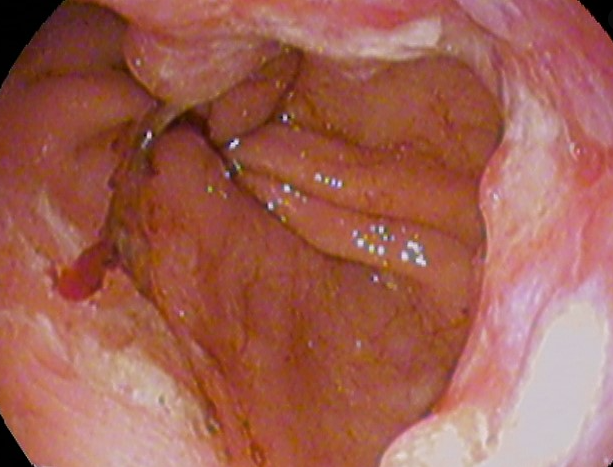
- Esophagogastroduodenoscopy (EGD) with biopsy
- Will show inflammation of the esophagus
- Doesn't diagnose the source
- 24 hour pH monitor

- Symptoms are logged by the patients
- If the symptoms overlap with low pH = GERD
- Esophagogastroduodenoscopy (EGD) with biopsy
- Esophageal manometry
- Measures the closing pressure of the LES to diagnose incompetence
- Not used as commonly anymore
- Important if surgical management is planned
- PPIs for 6 weeks
- If red flags present
- Red flag symptoms
- Swallowing difficulty
- Nausea/Vomiting
- Anemia
- Weight loss
- Diagnosis
- EGD first to rule out neoplasia
- Red flag symptoms
Treatment
- If the PPI and lifestyle modifications work, this means GERD is diagnosed
- The current management should be continued for a lifetime
- Esophagitis (without malignancy or metaplasia) seen on the EGD:
- Managed the same way with starting the patient on PPIs and lifestyle modifications
- If there is metaplasia from the EGD biopsies:
- High dose PPI management should be started
- Regular surveillance EGD's need to be done to make sure recurrence does not occur
- Every ~3 years
- If there is dysplasia on biopsy:
- Local ablation
- Cryotherapy
- Radiofrequency ablation
- Laser ablation
- High dose PPIs
- Regular surveillance EGD's need to be done to make sure recurrence does not occur
- ~1 year or more frequently
- Untreated dysplasia>adenocarcinoma
- Local ablation
- If there is adenocarcinoma
- Resection
- Staging
Surgery
- Nissen fundoplication
- Superior stomach wrapped around itself
- Usually done if the patient cannot tolerate or does not want to take PPIs
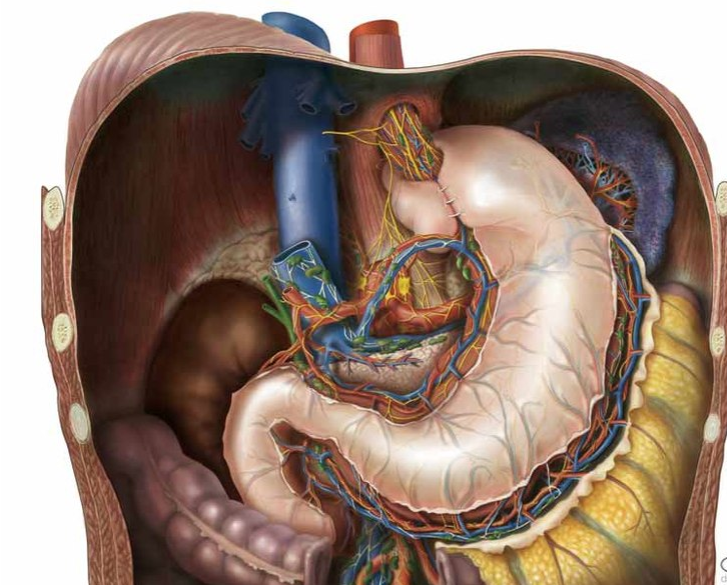
- Can have complications of surgery and can lead to achalasia
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.
