Gestational diabetes mellitus (GDM)
The presence of a fetus during pregnancy makes the maternal body more resistant to insulin and reduces peripheral tissue glucose uptake. This ensures that the fetus gets a continuous supply of glucose for itself. The result of these 2 factors means that 3-5 percent of pregnant mothers will experience gestational diabetes mellitus (GDM).
Maternal complications
Fortunately, the risk of GDM to the mother is low, with no risk of DKA (common in type 1 DM). However, women who have GDM are at a higher risk for GDM during a subsequent pregnancy (50%) and to developing diabetes after pregnancy (40-60%).

Fetal complications
The biggest fetal complication of GDM is macrosomia (large fetus) leading to a c-section. The cause of this is the mothers high blood sugar passing to the fetus and being converted into fat.

Screening guidelines
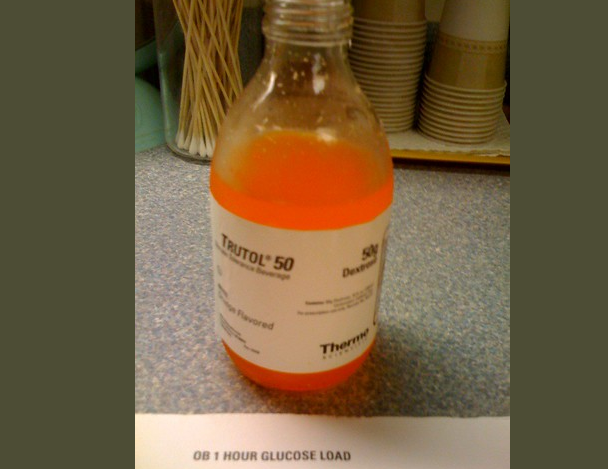
In the US all women are screened with the glucose load test (GLT) at 24-28 weeks. Women with risk factors such as previous GDM, obesity, macrosomia, unexplained fetal demise are screening twice, once at 16-20 weeks and again at 24-28 weeks. The GLT a nonfasting GDM test that involves the consumption of 50g glucose with a venous blood sample 1 hour later. If the glt is positive (GLT>7.8) a glucose tolerance test (GTT) will need to be completed. GTT involves the consumption of 75g glucose with a venous blood sample 2 hours later. Fasting glucose >5.5 and GTT of >7.9 at 2 hours will confirm GDM. Keep in mind that there are other cut-offs with their own positive predictive values and false positives.
Management
The management of GDM for the mother involves tight blood glucose control (fasting >5.2, post prandial <7.8) in order to avoid macrosomia and its complications (C-section). Control via diet involves the consumption of a diabetic diet. If the fasting blood glucose level is >5.2, the mother will require medical treatment with insulin or other oral hypoglycemic. All women with GDM require a 75g GTT 6-8 weeks after labour, given their high risk for developing diabeets after GDM.
For the fetus, the ultimate complication would be macrosomia requiring a c-section as mentioned above.

Pregestational diabetes
This condition is the presence of classic type 1 and type 2 diabetes mellitus even prior to the pregnancy. Unlike GDM, there are significant consequences to the mother and the fetus.
Management
The management of pregestational diabetes should begin before pregnancy to avoid growth abnormalities and abortions. In general, the degree of diabetes control correlates with the rates of spontaneous abortions. HbA1c is used to monitor maternal diabetic control over the long term (past 3-4 months). The HbA1c value is checked before conception, at the first prenatal visit and then every 4-6 weeks.
With excellent diabetic control, these pregnant women can await spontaneous labour at term, however, to reduce the risks of fetal demise labour should happen no later than 40 weeks. An elective c-section should be planned in advance if the baby's weight exceeds 4500g.
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.
