Hypertensive Crisis
Definition
Severe elevation in blood pressure (SBP >=180mmHg or DBP >=120mmHg) with or without end-organ dysfunction

Categories
Hypertensive Urgency:
- BP elevation without end-organ dysfunction
- Can still be associated with headache, dyspnea, epistaxis, palpitations, anxiety
- Largely a consequence of inadequate HTN treatment or non-compliance
Hypertensive Emergency:
- BP elevation with end-organ dysfunction
- Evidence of damage to the retina, kidneys, heart, arteries and/or brain
Gestational Hypertensive Emergency:
- Severe HTN persisting >15mins plus end-organ dysfunction.
- Severe preeclampsia, eclampsia, hemolysis, elevated LFTs, low platelets (HELLP) syndrome
Pseudo Hypertensive Crisis:
- Transient BP elevations from external stimulus
- Pain, anxiety, stress, urinary retention, BP measurement errors
- NO end-organ dysfunction
- White-coat hypertension (see below)

Epidemiology
Most Affected Population:
- Elderly
- African Americans
- Men
- Patients with new or rapid BP elevation
- More susceptible to end-organ dysfunction at lower BPs because they haven't had chronic compensation/adaptation
Prevalence:
- 1-2% of general HTN patients
- Up to 11% of HTN patients admitted to hospital
- Up to 0.5% of all ED visits
- Pseudo-hypertensive crisis ~35% of inpatient HTN crisis, 91% outpatient HTN crisis
Etiology
Risk Factors for all HTN crisis:
- CHF, CAD, CKD, DLD, DM, Stroke, prior HTN
Causes:
- Primary HTN
- Medication non-compliance
- Inadequate treatment
- Secondary HTN
- Renal artery stenosis
- Arteritis
- Kidney pathology (think pre-renal, intra-renal, post-renal!)
- Endocrine
- Pheo
- Cushing
- Hyperaldo
- Renin tumour
- Hyperthyroid
- Carcinoid
- Obstructive Sleep Apnea
- Think hypoxia causing erythropoiesis, more RBCs in the blood raises BP
- Coarctation of the aorta
- Alcohol withdrawal
- Drugs!
- Medications (withdrawal from anti-HTN meds, especially beta-blockers)
- Recreational (cocaine, SSRI serotonin syndrome, etc.)
- Pregnancy
- Pre-eclampsia and eclampsia
- Neurogenic (head injury, infarction, hemorrhage, tumour)
- Acute stress
- trauma, burns
- Pain
- Guillian-Barre Syndrome
Clinical Presentation
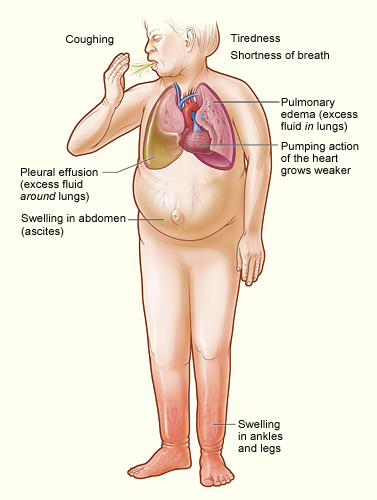
Complaints:
- Pulmonary edema (23%)
- SOB, WOB, cough, orthopnea
- Heart failure (12%)
- Chest pain, dyspnea, palpitations
- Headache
- Neurological Deficit
- Seizures
- Asymptomatic (common)
Ask about:
- Duration of prior HTN
- Recent BP measurements
- Cardiovascular risk factors
- Comorbidities
- Neuro symptoms
- headache, nausea, vomiting, weakness, numbness, tingling
- visual disturbance!
- Cardio/resp symptoms
- SOB, orthopnea, cough, fatigue
- Sleep apnea
- Diaphoresis (pheo?)
- Dysphagia (Guillian-Barre?)
- Urinary hesitancy
- Red flag headache symptoms (SAH?)
- Sudden onset, worst headache ever
- Red flag chest pain (aortic dissection?)
- Sudden onset, severe pain radiating to the back
- Drug Use
- Prescription (e.g. anti-HTN, erectile dysfunction meds), OTC (e.g. NSAID), herbal, recreational (e.g. cocaine)
Physical Exam:
Step 1: Confirm BP yourself with properly fitting cuff! If a true crisis, inform SMR/staff ASAP!

Step 2: Assess for end-organ dysfunction

- Fundoscopy
- Retinopathy (above and left, compared to normal above and right), hemorrhages, exudate, papilledema
- Full neurological exam
- Unilateral signs uncommon without ischemic brain injury
- Mental status? Signs of encephalopathy?
- Vascular
- Pulses in all extremities vs. central
- Cardiac
- Rate and rhythm
- Murmurs
- Volume status and JVD
- PMI
- Is this patient in heart failure? (see below... keep in mind volume overload from other sources... nephrotic syndrome, cirrhosis, hypoalbuminemia, etc.)
- Abdomen
- Renal bruits?
- AAA?
- Head & Neck
- Carotid bruits?
- JVD?
- Head injury?
- Respiratory
- Wheezing?
- Crackles?
Diagnostic Testing
Blood Pressure & Heart Rate:
- >180/120 mmHg for hypertensive emergency and urgency
- Heart rate typically more elevated with hypertensive emergency
- This makes sense, compensation for dysfunctional perfusion of the end-organs that are being damaged!
- >160/110 mmHg for >15mins in pregnancy
End Organ Dysfunction:
- Physical exam!!
- ECG
- Myocardial ischemia
- Secondarily for getting a sense of LVH (chronicity, heart failure)
- BNP
- Heart failure
- CBC
- MAHA
- LFTs
- Liver dysfunction
- Chest x-ray or CT
- Pulmonary edema?
- Head CT
- Neuro ischemia
- Coagulation studies
- Liver dysfunction
- Also important for gauging risk of bleeding
- Creatinine
- Kidney dysfunction
Narrowing the Diagnosis:
- Urinalysis
- metanephrines (pheo)
- RBCs, protein, casts (renal dysfunction)
- Lytes
- Hyperaldosteronism?
- Bladder ultrasound
- Outlet obstruction
- Renal Ultrasound
- Artery stenosis (secondary HTN)?
- CT head
- Trauma? Ischemia? Hemorrhage?
- Echocardiogram
- Heart failure?
- Creatinine
Management
IV Fluids:
- ONLY if volume-depleted
- Give NS (0.9%) or Lactated Ringer's
- In order to avoid hypoperfusion or hypotension when anti-hypertensive therapy started
Anti-HTN Medication Principle:
- SLOW (high risk of hypoperfusion)
- <25% reduction in the first few hours (no more than 20% in the first hour)
- Exceptions!!
- Acute Aortic Dissection
- Target SBP <120mmHg within first hour and HR <60bpm
- This patient is bleeding from/into their largest artery and will die soon without aggressive treatment
- Ischemic stroke
- Consider TPA, management can be complicated
- Hypertensive encephalopathy
- Target MAP reduction of 20-25% immediately
- Acute cardiogenic pulmonary edema
- Immediately reduce SBP <140 mmHg
- Eclampsia, severe pre-eclampsia, HELLP
- Immediately reduce SBP to <160 mmHg and DBP to <105 mmHg
- Acute cardiogenic pulmonary edema
- Acute intracerebral hemorrhage (see below)?
- Acute Aortic Dissection

Hypertensive Urgency:
- Place patient supine for 30-45 minutes before drugs
- Oral anti-HTN commonly used to lower BP to <160/95 in the first 48 hours.
- Nicardipine 20-40mg po q8-12h
- Captopril 25-50mg po q8-12h
- Labetolol 200mg po, then 200-400mg po q6-12h
- Close monitoring!!
Hypertensive Emergency:
- This patient needs to be in the ICU
- IV anti-HTN
- Nicardipine 5mg/hr and titrating up
- Sodium nitroprussied 0.3-0.5mcg/kg/min titrating up
- Labetolol 0.3-1mg/kg slow injection then boluses
- Esmolol 500mcg/kg over 1 minute then continued infusions
- Consider arterial catheterization for accurate BP measurements
- Manage the end-organ damage!
- BP targets and meds change depending on concurrent ACS, perioperative HTN, renal failure, preeclampsia, etc.
- Transition to oral anti-HTN as soon as stable and tolerating PO meds
Prognosis
Overall mortality ~3.7%
- ~4.6% in HTN emergency
- ~0.8% in HTN urgency
Citation, and more information available at:
DynaMed [Internet]. Ipswich (MA): EBSCO Information Services. 1995 -. Record No. T114059, Hypertensive Crisis; [updated 2018 Nov 30, cited 2020-Aug-05]. Available from https://www.dynamed.com/topics/dmp~AN~T114059. Registration and login required.
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.
