Mesenteric ischemia
There are 3 major mesenteric arteries (2 shown in the diagram below): Celiac trunk, superior mesenteric artery, inferior mesenteric artery
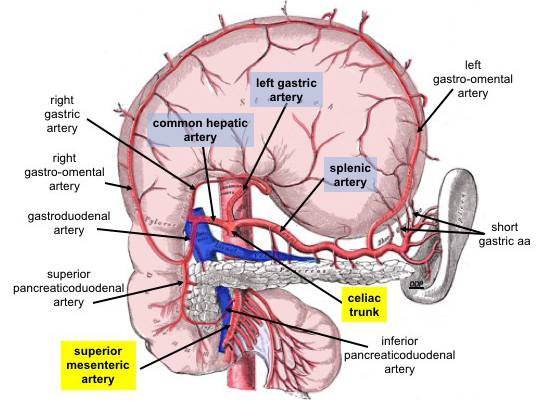
Diagram 1. Celiac trunk, SMA and IMA are the 3 major vessels supplying the abdominal organs
Mesenteric ischemia involves the occlusion or significant stenosis of at least 2 of these. Arterial mesenteric ischemia makes up the majority (~80%) of mesenteric ischemia cases, but can also be caused by the venous system (15%) and even be caused by non-occlusive disease.
Arterial mesenteric ischemia
- Chronic
- Usually caused by stenosis at the mesenteric artery root
- Mesenteric flow is intermittently or chronically reduced
- Presentation
- Postprandial abdominal pain = "mesenteric angina"
- Food avoidance and weight loss can be seen = small meal syndrome
- Diarrhea or steatorrhea due to malabsorption
- Risk of vitamin deficiency (especially fat-soluble ones- A,D,E,K)
- Workup
- Duplex U/S scan
- Blood flow velocities are monitored
- Angiography via CTA, MRA
- Gold standard but invasive
- Duplex U/S scan
- Management
- Endovascular
- Angioplasty and stenting
- Usually, one of the vessels are treated (ideally SMA)
- Acute thrombosis and dissection are risk factors
- Open surgical
- Patch angioplasty
- Widens the stenosis area
- Bypass grafting
- Antegrade
- From other mesenteric artery or the aorta
- Retrograde
- From the iliac arteries
- Antegrade
- Patch angioplasty
- Endovascular
- Acute
- Sudden occlusion of one of the mesenteric vessels
- ~60 minutes or greater time will lead to the infarction of the small bowel and require surgical resection = short bowel syndrome = <200cm viable small bowel

- Dead bowel, shown above
- Mortality is north of 80%
- Presentation
- Non-specific abdominal pain
- Vomiting and diarrhea are common features
- Peritonitis and systemic sepsis are very late signs, indicating irreversible ischemia
- Pain is generally described as our of proportion
- Workup
- A high degree of clinical suspicion is required for diagnosis
- Non-specific inflammatory markers such as ESR and CRP can be elevated
- Additionally, lactate and acidemia will be seen once bowel hypoperfusion starts to turn into infarction
- CTA will show the occlusion
- Mesenteric angiogram is the gold standard but impractical
- Management
- ABCDEs, including hemodynamic instability
- Broad-spectrum antibiotics
- Anticoagulation not very effective since the timeline to mortality is very short
- Laparotomy for bowel resection and embolectomy
- Endovascularly, catheter-directed thrombolysis or suction embolectomy can be attempted
- Acidosis will get worse before getting better due to reperfusion
- Total bowel necrosis will require a surgical closure and palliative care for the patient (not compatible with life)
- Acute-on-chronic
Median arcuate ligament syndrome
This is a rare condition where the median arcuate ligaments just inferior to the diaphragm compress the celiac artery during inspiration, causing the signs and symptoms of mesenteric ischemia. Due to the nature of this condition, food avoidance and weight loss will generally not be observed. Treatment is via surgery, and involves dividing these ligaments from the celiac artery
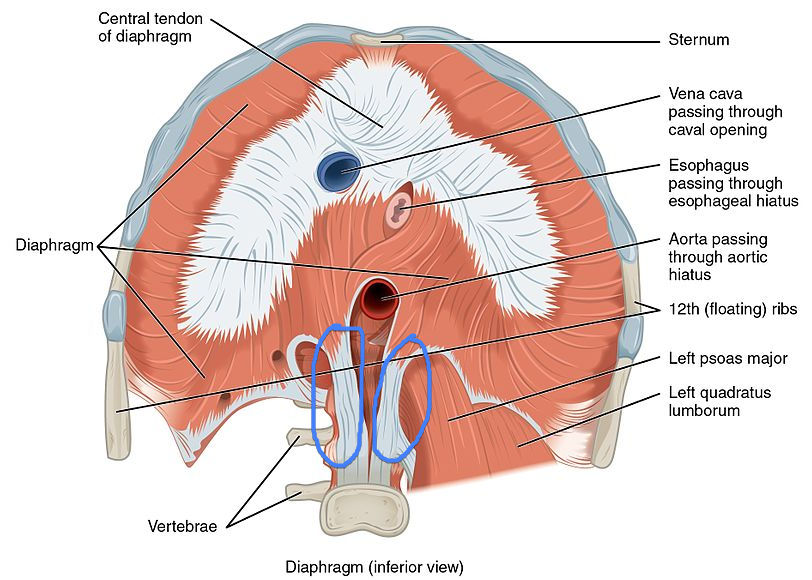
Diagram 2. Inferior view of the diaphragm. Highlighted in blue are the right and left crus of the diaphragm just lateral to the aorta.
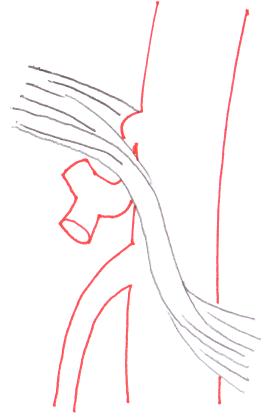
Diagram 3. Right crus of the diaphragm compressing the celiac trunk
Ischemia of the colon
Colonic ischemia occurs most commonly with problems of the inferior mesenteric artery. Watershed areas of the bowels include the areas that are at the margins of being supplied by 2 arteries. Watershed areas:
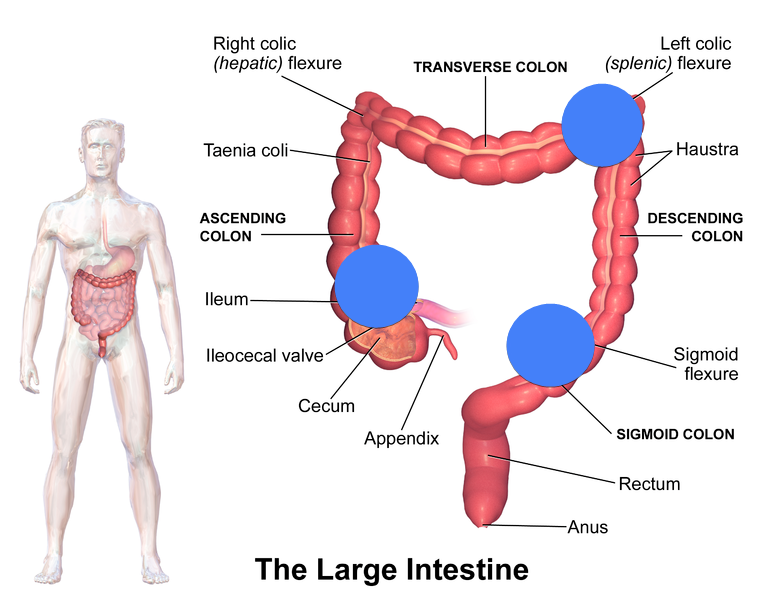
Diagram 4. Watershed areas of the bowel
- Splenic flexure - IMA and SMA
- Sigmoid colon - IMA and pudendal artery
- Cecum - Ileocolic and ileal artery
The ischemia seen in the colon can be anywhere from transient reversible ischemic colitis to total necrosis with high mortality.
- Causes
- Mostly atherosclerosis (95%)
- IMA occlusion in EVAR or open AAA repair
- Dissection
- Trauma
- Workup
- CTA
- Colonoscopy to visualize the watershed areas
- Can be useful only if there is late necrosis
- Mucose of the bowel will often be spared until the end
- Barium enema
- `Can show strictures formed from chronic ischemic colitis
- Management
- ABCDEs and broad-spectrum antibiotics
- Bowel necrosis, perforation or narrowing are indications for surgical management
- Revascularization of the remaining bowel can be attempted
- End colostomy and sub-total colectomy can be performed
- The rectum is usually spared because of dual blood supply from the inferior rectal artery from the pudendal artery (superior rectal artery comes from the IMA)
Venous mesenteric ischemia
This pathology essentially results from a deep vein thrombosis (DVT) but in the mesenteric veins. The severity of this condition can also range from non-occlusive to complete occlusion of the portal venous system. In 25% of the causes, the cause of thrombus is unknown.

Diagram 5. Portal vein thrombosis
- Causes - 75% of the time
- Malignancy - most common
- Cirrhosis
- Clotting disorders
- Presentation
- Asymptomatic
- Vague abdominal pain
- Sepsis
- Varicose vein bleeding
- Workup
- CTA
- Venous duplex scan
- Management
- ABCDEs
- Medical anticoagulation
- Thrombolysis is rarely done because of the risk of bleeding or bowel perforation
- Surgery reserved for complications such as perforation and necrosis
Non-occlusive mesenteric ischemia
Generally seen in critically ill patients with perfusion issues (think ICU). Because of systemic hypoperfusion, the "watershed" areas are affected the most. Inotropic agents, usually administered in order to increase or maintain cardiac perfusion can actually worsen mesenteric perfusion due to vasoconstriction. Mortality rates for these patients is very high, but that is mostly because they already have a high base level of mortality (~80%).
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.
