Postpartum hemorrhage
Postpartum hemorrhage is defined as a loss of 1L of blood during a C-section and a loss of 500ml of blood during vaginal birth which is close to the average amount of blood lost during each of these procedures. Postpartum hemorrhage can lead to hemorrhagic shock as depicted below.
| Class 1 | Class 2 | Class 3 | Class 4 | |
| Blood loss (ml) | <750 | 750–1500 | 1500–2000 | >2000 |
| Blood loss (%) | <15% | 15–30% | 30–40% | >40% |
| Pulse rate (beats/min) | <100 | >100 | >120 | >140 |
| Blood pressure | Normal | Decreased | Decreased | Decreased |
| Respiratory rate (breaths/min) | 14–20 | 20–30 | 30–40 | >35 |
| Urine output (ml/hour) | >30 | 20–30 | 5–15 | Negligible |
| CNS symptoms | Normal | Anxious | Confused | Lethargic |
Hemorrhagic shock can be tricky to diagnose in pregnant women due to their increased volume of plasma and red blood cells. This increase allows them to compensate and show little to no vital sign changes until they become hemodynamically unstable very quickly.
Types
- Early
- Within 24 hours
- Late
- Within 24hrs to 6 weeks
The 4 T's of PPH
There are 4+1 distinct causes of PPH.
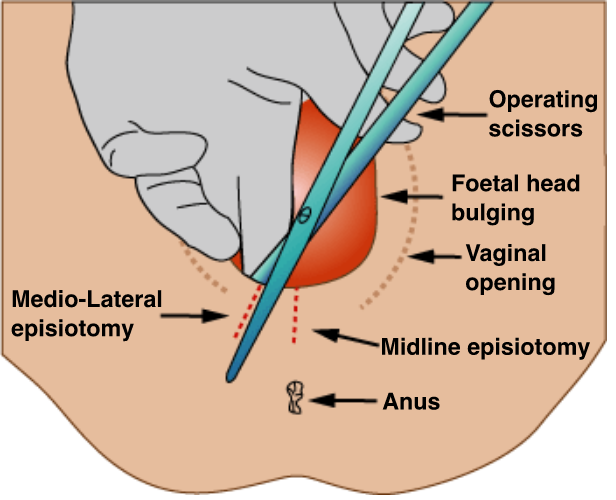
- Trauma
- The tone of the uterus will be normal/firm
- Vaginal or urethral lacerations
- Causes
- Episiotomy
- Macrosomia
- Perineal tear
- Episiotomy
- Management
- Put pressure
- Sutures to control the bleed
- If no clear source > Consider disseminated intravascular coagulation as a cause
- Thrombin = Clotting issues
- Von Willebrand disease, hemophilia a and b, anticoagulation medication, DIC
- Investigations
- Elevated INR
- Management
- DIC
- Administer platelets
- Red blood cells
- FFP
- DIC
- Tone = Atony of the uterus = most common cause
- The uterus needs to contract after delivery to allow all the blood vessels to close shut
- Sometimes this doesn't happen or doesn't happen efficiently
- Causes
- Tired uterus from prolonged labour
- Drugged uterus from tocolytics/anesthetics
- Stretched uterus from polyhydramnios, macrosomia, multiple gestations, fibroids
- Pathological uterus from endometritis, fever, chorioamnionitis
- Causes
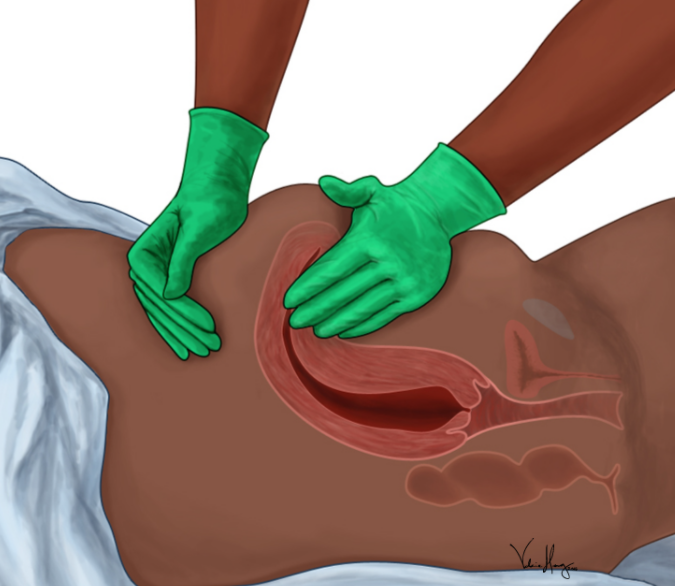
- Uterus feels boggy from the outside
- Management
- Fundal massage from the outside
- Medications
- Oxytocin
- Methergine
- Hemabate
- Fundal massage from the outside
- Tissue = retained placental parts
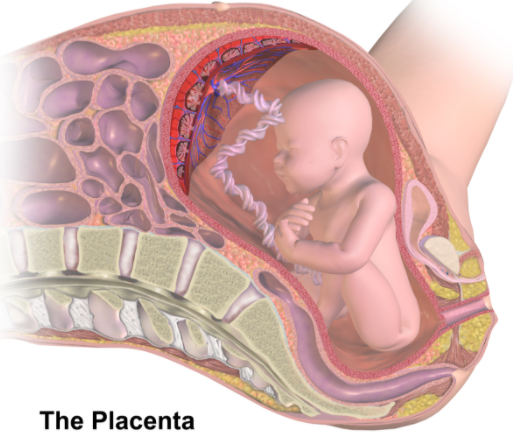
- Placenta buries itself deep into the endometrial tissue during normal pregnancy in order to get blood for the developing fetus
- Sometimes the placenta digs in too much
- Placenta accreta - in the endometrium, but deeper
- Placenta increta - in the myometrium but not the outside wall
- Placenta percreta - Through all the layers
- During labour, the placenta detaches from the wall
- If it is buried deep it the detachment will be incomplete and the retained placenta will keep delivering blood into the torn blood vessels
- These retained products need to be removed
- Management
- Dilation and curettage
- Can lead to a hysterectomy
- Track beta-HCG levels postpartum to ensure that there are no placental retention products
- Uterine inversion
- Uterus "births" itself
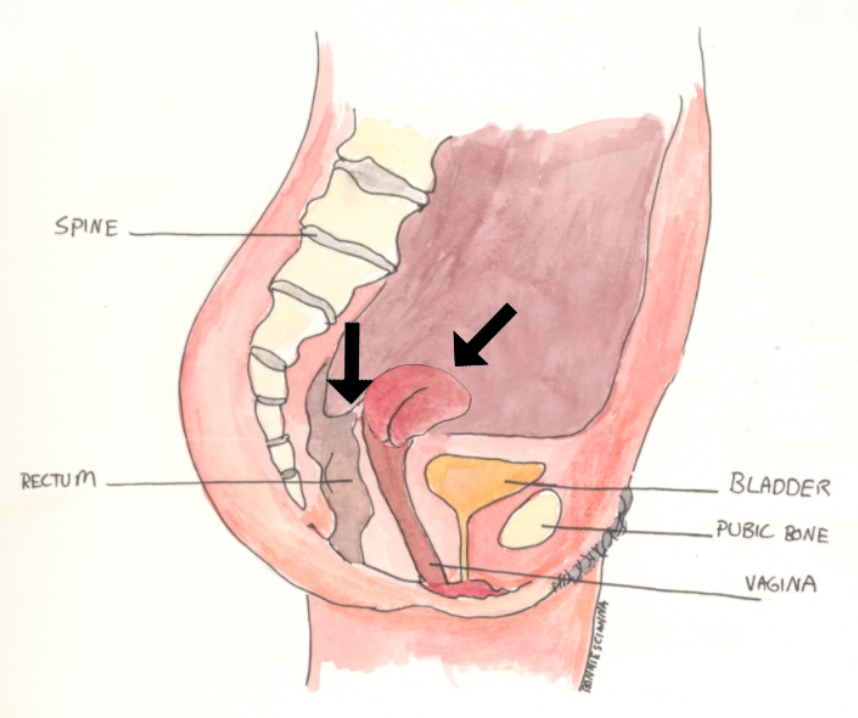
- Cannot palpate the uterus from the outside
- Causes
- Excess oxytocin use
- Manual pulling of the uterus
- Management
- Tocolytics to calm it down
- Put it back
- Give oxytocin to make it functional again
- Uterus "births" itself
Management with no identified cause
The vagina and the uterus make up an exposed cavity that has the ability to bleed a lot and bleed quickly. As such, if no obvious cause can be diagnosed and reversed a uterine bleed is treated the same way a GI bleed would be treated.
- 2 large-bore IVs (18 or higher)
- Fluids
- Transfuse blood as needed
- Surgery (OB) consult - if the patient is already in the OR
- Uterine artery ligation
- Total hysterectomy
- IR consult - if not already in the OR
- Uterine artery embolization
- IV estrogen can help but not if there are structural causes to the bleed
- TXA
- TXA will stabilize existing blood clots by competitively inhibiting the Lysine receptor found on plasminogen
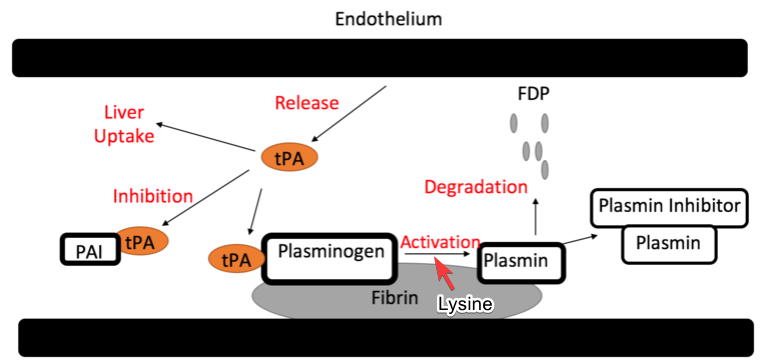
- Cannot give to patient with a PE/DVT
- No PPI obviously
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.