The Antibiotic Ladder
The antibiotic ladder is used to slow down the antibiotic resistance that the bacteria are developing. The idea is to use the weakest antibiotic that is sufficient to kill off the given bacterial colony. This way there is no generalized killing of all bacterium, leading to the formation of superbugs.
In general, going higher on the ladder means using newer antibiotics.
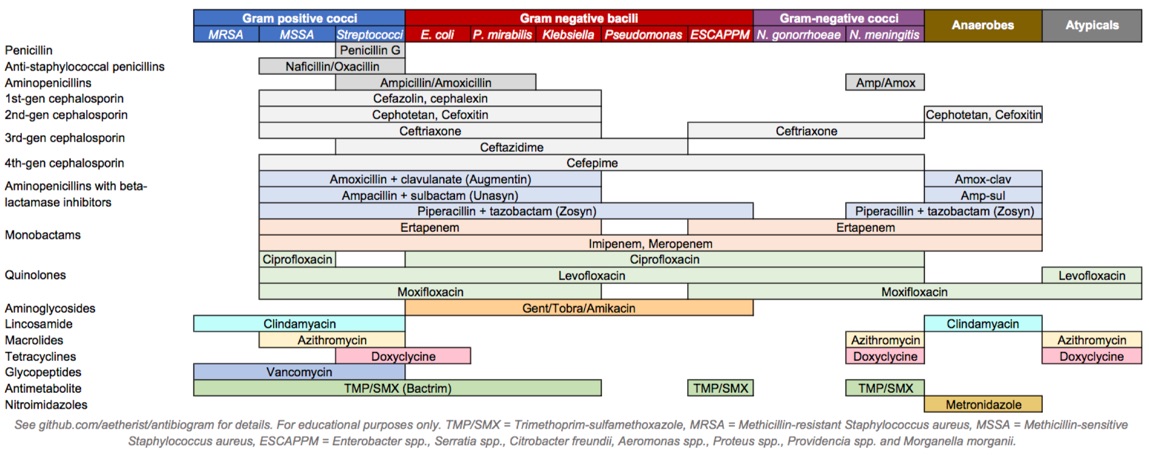
Diagram 1. Various antibiotics and their coverage.
- Penicillin
- The first antibiotic developed
- Lots of bacteria have developed resistance to this and currently, syphilis is one of the only organisms susceptible to penicillins
- Bacteria evolved to produce the beta-lactamase enzyme to break down penicillins
- We managed to develop new penicillins
- Aminopenicillins
- Designed for gram-negative bacteria
- Small in size to pass through the gram-negative bacterial wall
- The small size resulted in them being susceptible to beta-lactamase enzymes
- Examples
- Antibiotics that start with "Am"
- Ampicillin
- Amoxicillin
- Aminopenicillins in addition to beta-lactamase inhibitors
- Makes these resistant to beta-lactamases
- Can be used for gram positives
- Examples
- Amoxi clavulin
- Ampicillin sulbactam
- Anti-pseudomonal penicillins
- Only use if Pseudomonas is being treated despite a wide coverage
- These include beta-lactamase inhibitors as well
- Examples
- Piperacillin/Tazobactam (Piptazo)
- Ticarcillin/Clavulanate
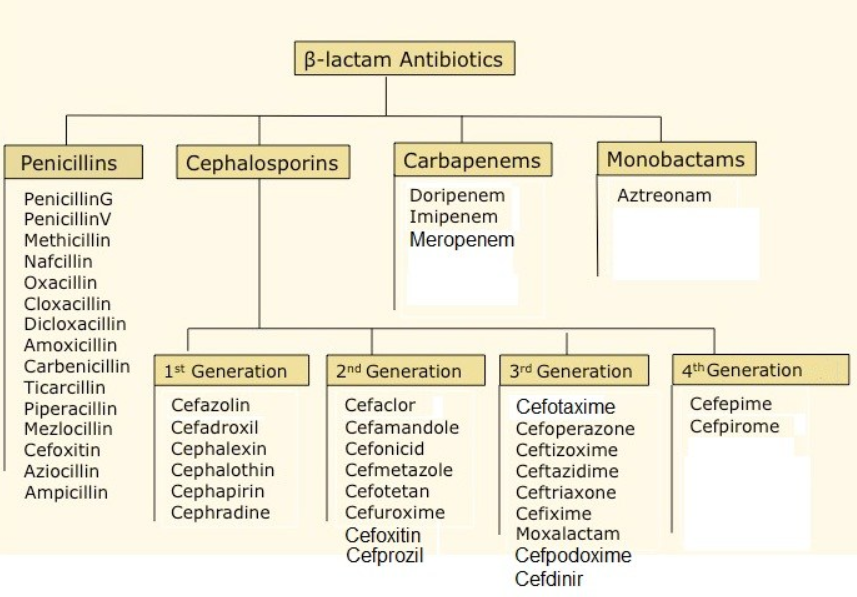
- Stronger anti-pseudomonal penicillins - Carbapenems
- Examples
- Meropenem
- Monobactam
- Aztreonam - used as first-line in severe penicillin allergy
- Examples
- Methicilin sensitive staph aureus (MSSA) antibiotics
- Examples
- Nafcillin
- Dicloxacillin - oral
- Examples
- Methicillin-resistant staph aureus (MRSA) antibiotics
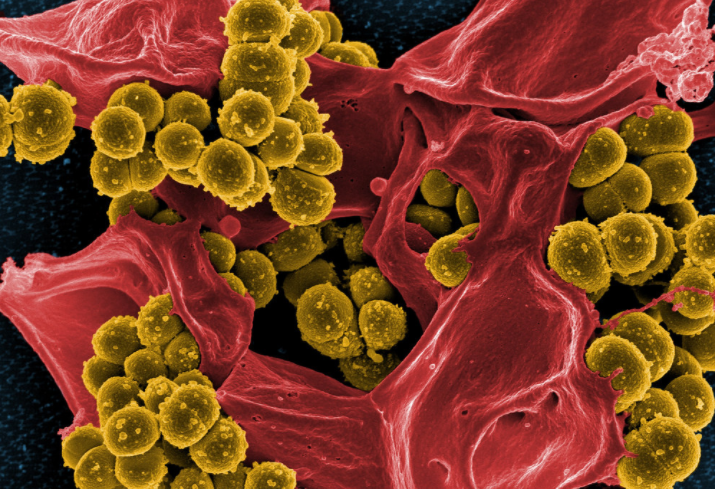
- Examples
- Vancomycin
- Used exclusively for MRSA
- Daptomycin
- Used to treat blood infections
- Doesn't work for lung infections
- Linezolid - L=lung
- Used to treat lung infections
- Doesn't work for blood infections
- Vancomycin
- Aminopenicillins
- Cephalosporins
- Generations
- 1st
- Work really well on gram positives
- Not useful for gram negatives
- Used for skin infection prophylaxis or for the treatment of cellulitis
- Examples
- Cephalexin/Keflex
- Cefazolin /Ancef
- 2nd
- Not good for gram negatives
- Okay for gram positives
- 3rd
- Work better on gram negatives
- Also works on strep
- Examples
- Ceftriaxone
- 4th
- Examples
- Cefepime
- Used as an antipseudomonal
- Cefepime
- Examples
- 1st
- Generations
- Fluoroquinolones
- Examples
- Ciprofloxacin
- Used to treat gram negatives exclusively
- Used to be used for UTI's in the past - no longer works
- Currently used for Pseudomonas (double coverage)
- Levofloxacin
- If the bug is susceptible to levofloxacin, use levofloxacin before moxifloxacin
- Moxifloxacin
- Respiratory fluoroquinolone
- Used to treat gram-positive organisms such as strep (pneumonia bugs)
- Ciprofloxacin
- Examples
- Anti-anaerobes
- Examples
- Metronidazole
- Used in the gut and vagina for anaerobes
- Clindamycin
- Used in other places for anaerobes
- Metronidazole
- Examples
Antibiotic use principles
General antibiotic use dictates that sick patients get broad antibiotics. If patients are not getting better, multiple antibiotics are added. When trying to narrow the antibiotics a patient is on, remove the antibiotics one at a time. Doing this ensures that in the event that the patient gets worse after the antibiotic removal it is obvious which antibiotic needs to be put back on.
- Community-acquired pneumonia

- Ceftriaxone + azithromycin
- If hospitalized
- Azithromycin
- In the community
- Moxifloxacin
- Used if the patient is allergic to beta-lactams
- Pseudomonas and MRSA
- Vancomycin and piptazo
- Linezolid and meropenem
- If vancomycin and piptazo cannot be used (allergy)
- Meningitis
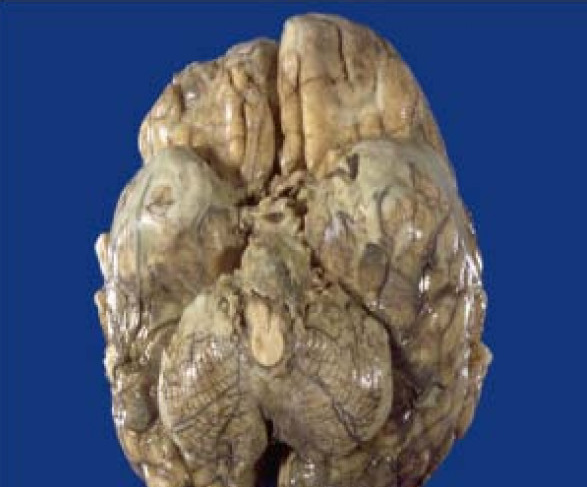
- Vancomycin + Ceftriaxone + steroids + ampicillin (if immunocompromised)
- UTI
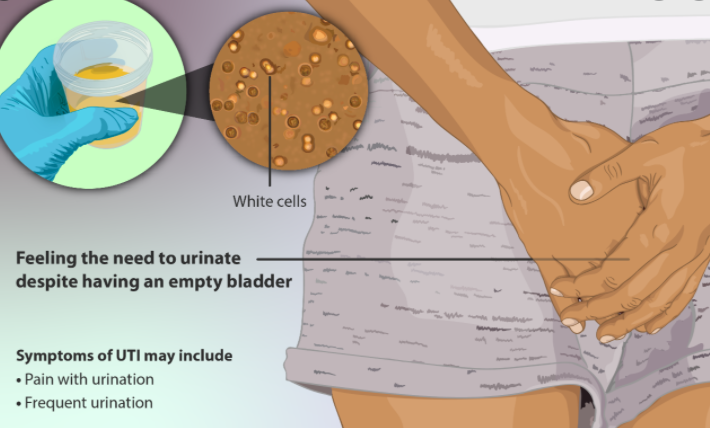
- Amoxycillin
- Best for outpatient
- Macrobid = Nitrofurantoin
- If allergic to beta-lactams
- Sulfamethoxazole and trimethoprim
- Worse than the 2 above
- Ciprofloxacin
- Not able to use this anymore
- Pyelonephritis
- Ceftriaxone
- Cellulitis

- Caused by strep
- Amoxicillin - outpatient
- Ceftriaxone - inpatient
- Caused by staph
- Clindamycin - outpatient
- Vancomycin - inpatient
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.
