Direct oral anticoagulants
The field of antithrombotic agents for patients requiring anticoagulation has truly been revolutionized in the last few decades.
Direct oral anticoagulants (DOACs) are known by various other names such as novel oral anticoagulants (NOACs), target-specific oral anticoagulants (TSOACs), oral direct inhibitors (ODIs). All of these terms describe the same oral anticoagulant agents highlighted above. Compared to traditional anticoagulation DOACs produce less bleeding, do not require bridging, can be taken orally, have short half-lives, and do not require monitoring. Reversibility of these agents can also be done more readily.
- Contraindications

- Pregnancy
- Breastfeeding/nursing
- Severe liver disease or failure
- Antiphospholipid syndrome
- Indications
- VTE
- DVT and PEs
- VTE prevention
- Post-surgery
- Atrial fibrillation
- Stroke prevention
- Acute coronary syndrome (ACS) prevention
- Usually not oral
- Heparin-induced thrombocytopenia management
- VTE
Traditionally anti-thrombotic agents include both antiplatelet and anticoagulation agents.
- Antiplatelets
- Inhibit platelet aggregation
- ASA
- Uses
- Primary or secondary prevention of cardiovascular disease
- Mechanism
- COX-1 inhibiton leading to decreased thromboxane A2 levels
- Affected platelets remain dysfunctional for the rest of their lifespan (7-10 days)
- 7-10 days ebfore full effect
- Caution
- Stop 7-10 days before surgery if required
- Uses
- Plavix/Clopidogrel
- Uses
- ACS, Stroke
- Mechanism
- ADP receptor inhibition = irreversible platelet activation inhibition
- Caution
- Administration with a PPI reduces effect
- Uses
- Dextran
- Uses
- IV antiplatelet agent
- Used after carotid endarterectomy and infrainguinal bypasses
- Mechanism
- Antiplatelet activity
- Decreased blood viscosity
- Uses
- Aggrenox
- Uses
- Secondary prevention in stroke
- Mechanism of action
- Thromboxane synthase inhibitor
- Half life
- 10 hours
- Caution
- Can cause GI and headaches
- Uses
- Thienopyridines
- Uses
- ACS
- Mechanism
- ADP receptor inhibition = irreversible platelet activation inhibition
- Uses
- Anticoagulants
- Agents that inhibit the coagulation cascade
- Holding
- 2-3 days prior to the procedure if no renal problems
- 2-4 days prior to the procedure if renal problems
- Can restart after the procedure at the same dose
- Types
- Direct thrombin inhibitors (DTIs)
- Parenteral forms
- Revasc
- Argatroban
- Can be used in HIT
- Angiomax
- Usedin unstable angina and angioplasty
- Oral
- Dabigatran/Pradaxa
- Indications
- Can be used in Afib instead of warfarin
- Mecanism
- Inhibits free and clot bound thrombin
- Half-life is 12-17 hours
- Mostly excreted through the kidneys (caution for kidney disease patients)
- No monitoring required
- Unaffected by food intake
- Do not use with prosthetic heart valves
- Reversal
- Activated charcoal to prevent absorption from the gut
- Hemodialysis
- Novoseven (factor 7a)
- Idarucizumab
- Indications
- Dabigatran/Pradaxa
- Parenteral forms
- Direct factor Xa inhibitors
- No IV forms!
- Holding
- 2 days prior to a low-risk procedure (colonoscopy, endoscopy)
- 3 days prior to a high-risk procedure (surgery)
- Oral
- Rivaroxaban/Xarelto
- Inhibits free and clot bound factor 10a
- Half-life is 5-9 hours
- Requires food intake (absorption will be reduced otherwise)
- No monitoring required
- Do not use in prosthetic heart valves
- Kidney function dependent dosing only for AFib
- Reversal
- Andexanet alfa
- Apixaban/Eliquis
- Inhibits free and clot bound factor 10a
- Half-life is 12 hours
- Unaffected by food intake
- No monitoring required
- Do not use in prosthetic heart valves
- Kidney function dependent dosing only for Afib
- Reversal
- Andexanet alfa
- Edoxaban
- Not used in North America
- Requires a 5-10 day period of parenteral anticoagulation first
- Inhibits free and clot bound factor 10a
- Half-life is 10-14 hours
- Unaffected by food intake
- No monitoring required
- Do not use in prosthetic heart valves
- Complete renal excretion
- Reversal
- Andexanet alfa
- Betrixaban
- Inhibits free and clot bound factor 10a
- Half-life is 19-27 hours
- No monitoring required
- Only use in hospitalized patients for VTE prevention
- Minimal renal excretion
- Reversal
- Andexanet alfa
- Rivaroxaban/Xarelto
- Others (traditional anticoagulation)
- Warfarin
- Heparin
- Low molecular weight heparin
- Direct thrombin inhibitors (DTIs)
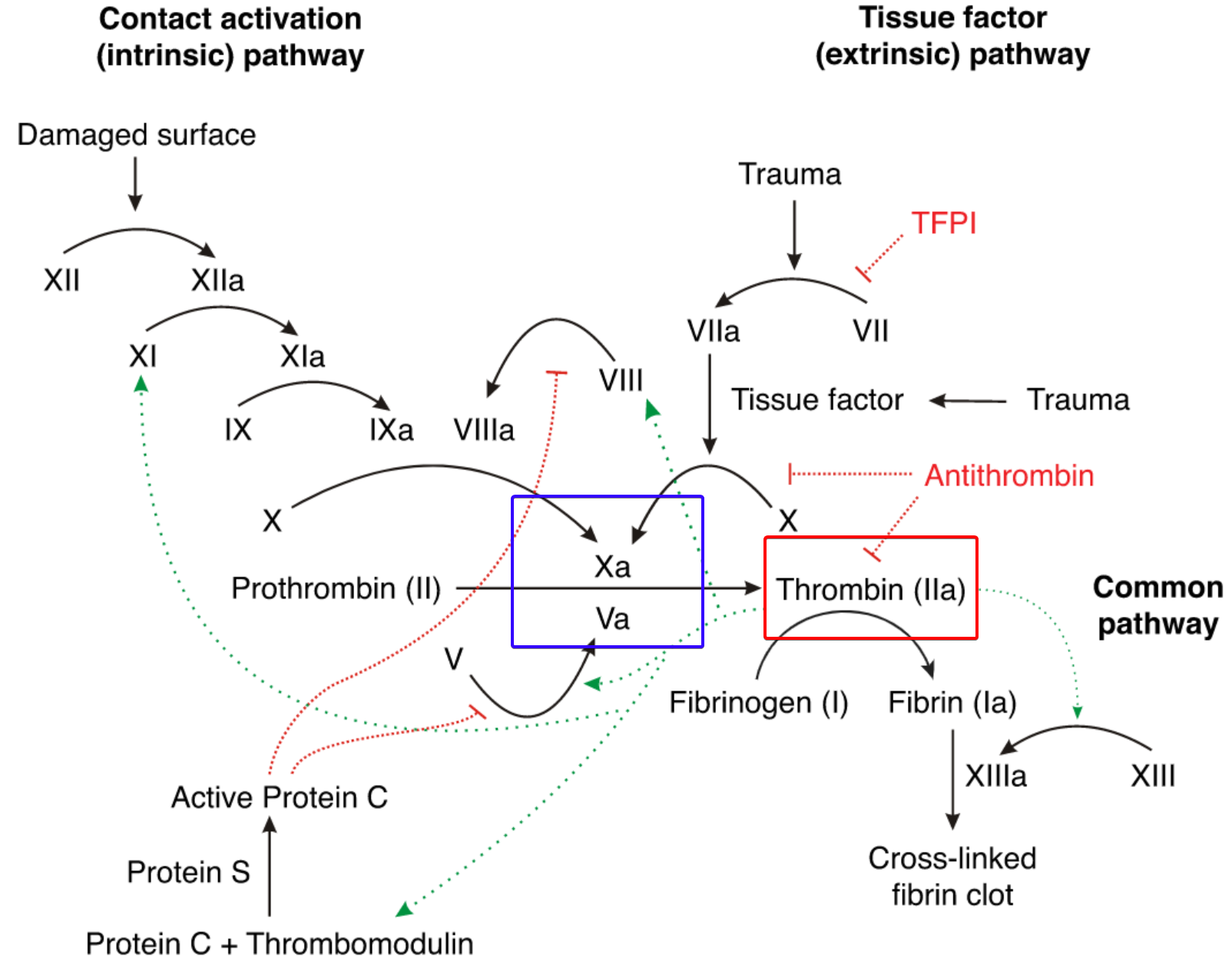
Diagram 1. Coagulation cascade. Direct factor Xa inhibitors act on factor Xa (blue square). DTIs act on thrombin (red square)
Traditional anticoagulation
- Heparin
- 2 types
- Unfractionated heparin (UFH)
- Mechanism
- Factor 10a inhibition
- Indications
- Cardiovascular anticoagulation
- DVT/PE
- Half life
- 1-1.5 hours
- Complications
- Heparin induced thrombocytopenia (HIT)
- Bleeding
- Reversal
- Protamine sulfate
- Mechanism
- Low molecular weight heparin (LMWH)
- Also known as enoxaparin injection
- Mechanism
- Factor 10 inhibition
- Indications
- Cardiovascular anticoagulation
- Venous thromboembolism prevention and treatment
- Contraindications
- Dialysis patients
- Must be dose adjusted if GFR<30
- Risk of bleeding less than UFH
- Small risk of osteoporosis
- Reversal
- Protamine sulfate less effective with LMWH than UFH
- Unfractionated heparin (UFH)
- Warfarin (oral)
- Mechanism
- Vitamin K inhibitor
- Inhibits factors 2, 7, 9, 10, protein C and S
- Takes effect after 3-5 days of daily administration
- Bridging
- In the first 3 days of warfarin therapy the levels of Protein S and C drop faster than the coagulation factors = Hypercoagulable state
- Need to administer LMWH for the first few days on warfarin
- Monitoring
- Requires INR monitoring (2<INR<3 to be therapeutic)
- Compliance issues with bw can be serious
- INR often supra/sub-therapeutic (above 3 or below 2)
- Reversal and half life
- Longer half-life
- Vitamin K reversal over hours-days
- FFP administration for quick reversal
- Mechanism
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.
