Stroke
Strokes happen when the brain cannot get enough blood to a part of the brain due to a vascular problem. There are 3 main types of strokes:
- Ischemic (2 subtypes) - 75% of the time
- Embolic
- Occlusion caused by something, not from the brain
- Causes
- Afib plaque
- Carotid artery plaque
- Vegetation from heart valves
- Risk factors
- Obesity
- Smoking
- Hypertension
- Dyslipidemia
- Diabetes
- Age
- Infection
- Thrombotic
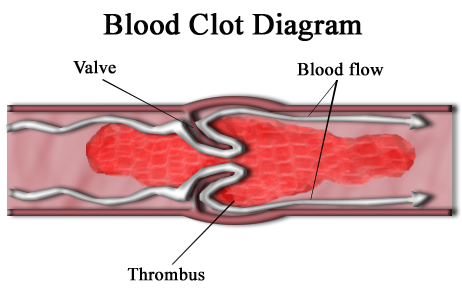
- Occlusion in the blood vessel
- Brain parts distal to the occlusion will die off
- Caused by a plaque (similar to an MI)
- Risk factors
- Obesity
- Smoking
- Hypertension
- Dyslipidemia
- Diabetes
- Age
- Embolic
- Hemorrhagic (intracerebral) - 25% of the time
- Poor outcome
- Will require a neurosurgeon
Pathophysiology
Strokes can affect one or multiple of the arteries within the circle of Willis.
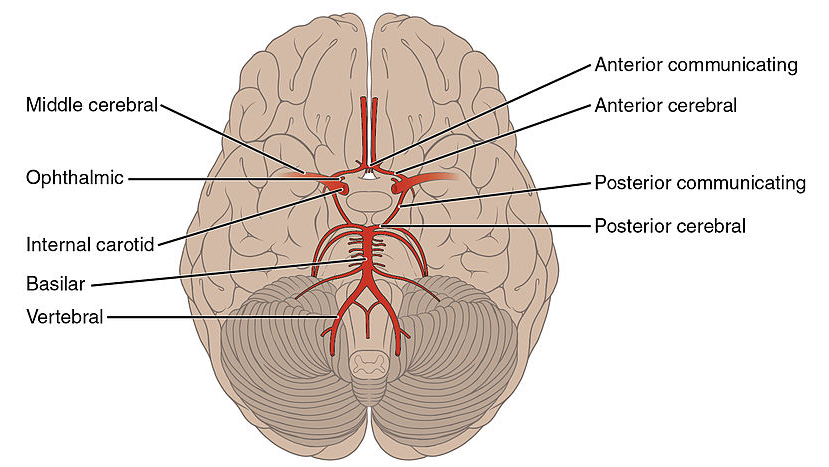
- Anterior cerebral artery (ACA)
- Lower limbs
- Middle cerebral artery (MCA)
- Upper limbs
- Face
- Speech
- Posterior cerebral artery (PCA)
- Visual cortex
- Balancing
- Syncope
Patients who end up with strokes tend to have common presentations. These are the following:
- Vasculapaths
- Patients with afib
- Often not on anticoagulation
- Young women post-trauma
- Neck pain with a focal neurologic concussion
- Patients with a thunderclap headache
- Worst headache of life with sudden onset
- Sometimes seen with Cushing's syndrome
- Bradycardia
- Hypertension
- Herniation soon to follow
Management
When a patient suspected to have had a stroke presents to the ED the first test that is needed is a non-contrast CT scan of the brain. This scan is quicker than contrast CT and helps to see blood. If blood is seen on CT, then this is a hemorrhagic stroke. If there is no stroke, then this is an ischemic stroke.
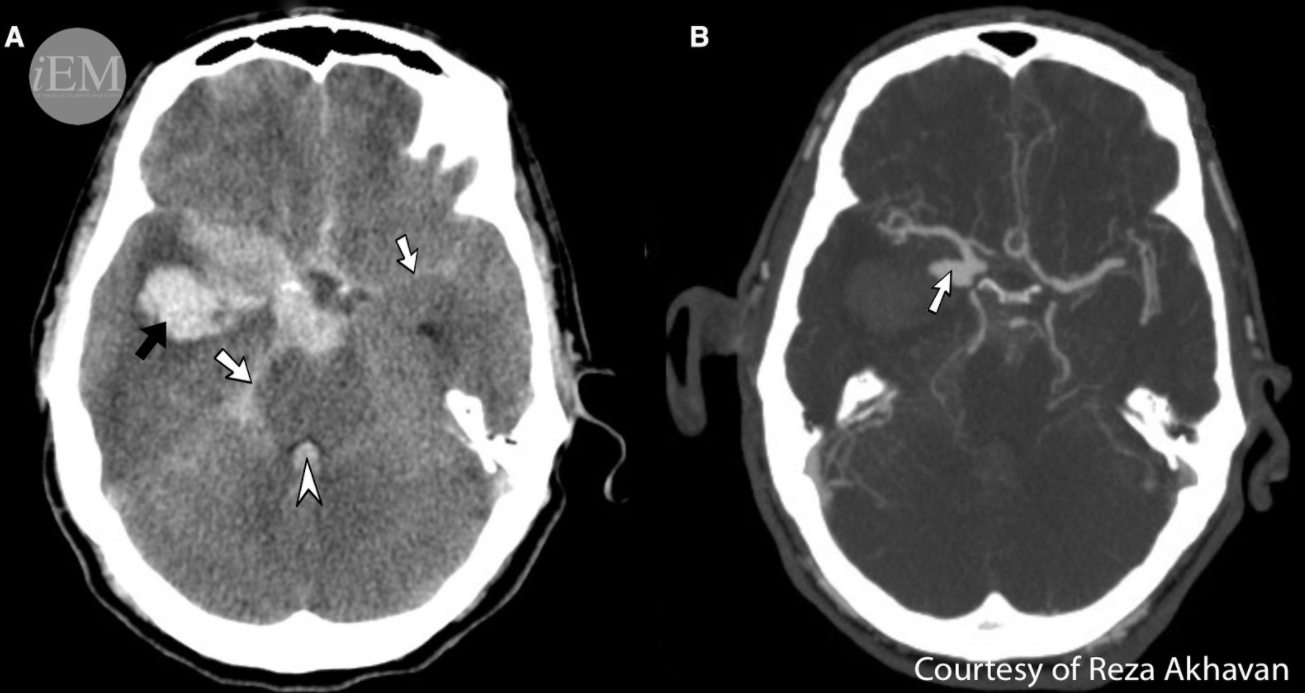
Picture 1. Intracranial hemorrhage on a non-contrast CT brain
- Hemorrhagic stroke - poor outcome
- Lower blood pressure
- Call neurosurgery
- Endovascular hemorrhage
- Clip
- Craniotomy - remove the skull to reduce the intracranial hemorrhage
- Administer free frozen plasma
- Only helps if the INR is high
- Ischemic stroke
- tPA
- Used to dissolve clots
- Indications
- Non-hemorrhagic stroke newer than 3 hours for diabetics, 4.5 hours for non-diabetics (neurologists can override these)
- Time starts from last time seen well (if you slept at 10 pm, by morning time no tPA)
- Contraindications
- Previous hemorrhagic strokes
- Risk of bleeding (watch for GI bleeds)
- Less than 2 weeks from a surgery
- Acute management if no tPA
- Antiplatelets
- ASA 325mg
- Control of diabetes
- Avoid hypoglycemia especially
- Permissive hypertension
- 220/120
- Maintains tissue perfusion in the brain
- Antiplatelets
- Chronic management
- Low molecular weight heparin
- Anticoagulation if afib or aflutter present
- ASA 81 daily and possible add dipyridamole
- High potency statins
- Atorvastatin
- Rosuvastatin
- Hemoglobin a1c should be under <8%
- Control blood pressure
- Lifestyle changes
- Stop smoking
- ECG/Telemetry/Holter monitoring
- Check for arrhythmias
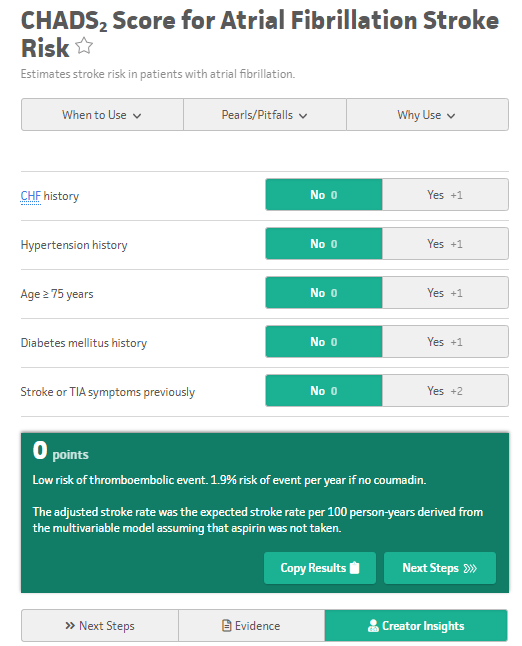
- Afib or aflutter
- This means a CHADs2 score of 2 or higher
- Anticoagulation
- Warfarin
- No need to bridge with heparin
- NOACs
- This means a CHADs2 score of 2 or higher
- Transthoracic echo
- Thrombus can be seen
- Warfarin
- Will need a heparin bridge
- NOACs
- Warfarin
- Thrombus can be seen
- Carotid U/S
- Carotid artery stenosis
- If stenosis <70% with no symptoms
- Treat medically
- If stenosis >80% or greater than 70% stenosis with symptoms
- Carotid endarterectomy (within 2 weeks) or stenting (for sicker patients)
- tPA
All information provided on this website is for educational purposes and does not constitute any medical advice. Please speak to you doctor before changing your diet, activity or medications.